Introduction
Intravaginal foreign body retained for long duration can be a diagnostic dilemma. The presenting symptoms may be persistent vaginal discharge, chronic pelvic pain, post menopausal bleeding. Diagnosis is based on radiological findings on USG /MRI. This report presents the case of a unmarried 18 year old who had an intravaginal foreign body for unknown duration, leading to vaginal stenosis,adnexal masses and haematocolpos.
Case Report
An18 year old unmarried woman was referred to gynaecologist with chronic pelvic pain of 2 to 3 years duration which was continuous, dragging in type and severe enough to interfere with her daily activities. There was no disturbance in bladder or bowel habits. Patient attained menarche at 13 years of age and is having regular menstrual cycles with scanty flow of 5 days duration, associa ted with pain.
On examination patient was afebrile, with mild anaemia, and stable vitals. Per abdomen no masses were palpable. There was tenderness in the suprapubic region. On per vaginal examination there was a blind vagina of 4 cm depth. The cervix could not be visualized. Per rectal examination a bulge was felt through the anterior rectal wall, 4cm above the anal opening with a boggy feel.
USG was done and showed
Uterus 5.6X3.6X2.7cms, endometrium 2mm,Rt ovary 6.2X 3.2cm with dominant follicle of 2.7 cm. Left ovary 3X 3.7 cms with multiple follicles. Lower uterine segment two echogenic streaks measuring 4mmX 1mm are seen.
Report : ?foreign body.
An MRI was done and reported as
1.Bilateral enlarged ovaries with prominent follicles and small pocket of right periovarian collection.
Likely possibilities are --b ilateral tubo ovarian masses / bilateral oophoritis.
2.Bulky cervix with heterogenous lesion in cervical canal with hypodense rim and having nodular enhancing component at its left lateral aspect and surrounded by fluid.
?nature ?foreign body
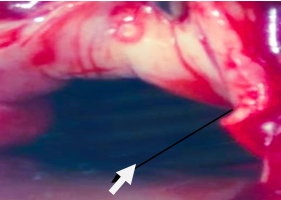
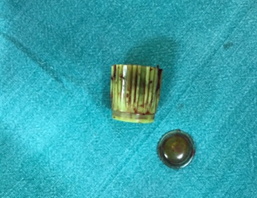
The patient denied any history of accidental or intentional insertion of a foreign body into the vagina. She was posted for examination under regional anaesthesia and procedure. A transverse vaginal septum was seen around 5 cm from the introitus. There was an opening admitting an uterine sound which could be passed for 2 cm length before encountering resistance. The opening in the septum was widened and by blunt and sharp dissection the space above the septum was opened under guidance of a finger placed in the rectum. The area was well vascularised and plane of separation was difficult to obtain. Even after dissecting for a distance of 5 – 6cm the fluid collection around the cervix could not be approached and rectal wall thinning was seen. It was decided to do a laparotomy to better visualize the anatomy and approach to the collection of fluid in the upper vagina. The abdomen was opened by a Pfannensteil incision. The uterus and adnexa were densely adherent to each other with indurated and fixed parametrium. The small bowel was adherent to the posterior wall of the uterus. The bladder was dissected off the vagina by sharp dissection and a transverse opening of 1cm was made into the upper anterior vagina l wall. Approximately 300ml of chocolate colored thin fluid was aspirated, leaving a closed space in the upper vagina. A finger introduced into this area felt a hard, rough object which was extracted by holding with artery forceps. It was found to be a 2 inches bottle cap. Cervix of 1.5cm length was palpated. Under guidance of a finger placed in the upper vagina, the vaginal dissection was completed and a continuous vaginal canal was obtained. The epithelium of the upper vagina was mobilized and could be brought down to the area of the divided septum and sutured with interrupted sutures. The rectal wall was sutured in two layers.
The opening in the upper vagina was closed. Purulent discharge of 20ml was drained from the right adnexal area. No further surgery was attempted and the abdomen was closed with a drain in the pelvis.
Daily insertion of a moist pack after gentle irrigation of the vaginal cavity was done for 7 days post operative. The patient was examined 4 wks after surgery. The vaginal canal was patent in its whole length and the cervix was visible.
Discussion
This is a rare case of a foreign body inserted into the vagina resulting in vaginal stenosis, haematocolpos and adnexal masses due to PID. The lower end of stenosed area had even undergone epithelialisation and looked like a septum. Menstrual blood was draining in small amounts through a small opening in the septum, with some collecting superior to the stenotic area of the vagina leading to haematocolpos.
Due to the distensibility of the vagina foreign body insertion does not usually cause pain. Objects with sharp edges may produce bleeding. Foreign body insertion in premenarcheal girls usually presents as foul smelling vaginal discharge which is not responsive to antibiotic treatment.1 Sexual abuse should also be ruled out.2 Forgotten tampons, can sometimes be retrieved from the vagina in adolescent girls and have been known to cause life threatening septic shock syndrome. Few cases of vaginal stenosis following long standing foreign body in the vagina have been described where the presentation was with persistent foul smelling vaginal discharge, sometimes blood stained3 Nakib et al retrieved a battery which was embedded in the vaginal wall by forcible dilatation under colposcopic guidance.4
Various objects have been inserted into the vagina to retain a prolapsed uterus, such as plastic bangles, wadded bits of cloth and hard fruit like wood apples (botanical name Limonia acidissima). Wood apples are hygroscopic and swell to distend the vagina and act like a space occupying pessary. Obstetric forceps application to the wood apple for dislodgement and removal has been described.5 Long standing vaginal pessaries used for retaining the prolapsed uterus have presented with foul smelling vaginal discharge and bleeding leading to the erroneous diagnosis of vaginal or cervical malignancy. Foreign bodies leading to vesico vaginal fistulae, or intraperitoneal migration have also been described in the literature.6
Metallic objects can be detected by pelvic X –Ray, or USG exam.7 Plastic and wooden objects may not produce a shadow. MRI examination offers the best opportunity to identify vaginal foreign bodies providing details of the degree of their penetration into adjacent bladder, rectal or parametrial tissues.8
In the present case persistent abdominal pain led the patient to seek medical assistance. She was diagnosed to have bilateral adnexal masses on USG and as patient denied history of sexual exposure a diagnosis of genital Tuberculosis was entertained and she even received a short course of anti TB drugs with no relief of pain or decrease in size of the masses. A second USG raised the suspicion of foreign body. In the presence of dense fibrotic tissue extending to the upper half of vagina, as in this case, an abdomino –perineal approach allows identification of dissection planes and injury to bladder and rectum can be avoided. If the vaginal epithelium cannot be mo bilized, or is not sufficient to cover the raw surface of the dissected vagina, a vaginal stent made of a condom filled with poly urethane foam and covered with split skin graft can be used to epithelialise the vagina.9 The patient will have to use vaginal dilators in the post operative period to prevent restenosis and maintain patency till epithelial cover is established.
MRI is regarded as the best technique for evaluating vaginal foreign bodies in young children. However, it is not always available or necessarily conclusive. Vaginoscopy with 4 mm hysteroscope under general anesthesia is very useful for detection and treatment of vaginal foreign bodies, especially in children11, 10 Hymen integrity can be preserved with this procedure.
Conclusion
Vaginal discharge in women of all age groups may be due to variety of causes. Persistent or recurrent vaginal discharge in prepubertal girls should raise the suspicion of vaginal foreign body. Vaginoscopy using a 4mm hysteroscope can help diagnosis and retrieval of the foreign body in young children. Intravaginal foreign body retained for long duration can be a diagnostic dilemma and as in the above case, prove difficult to remove. The recommended surgical approach for foreign bodies in the upper vagina obscured by dense vaginal adhesions is by combined abdomino-perineal approach to aid in dissection and prevent injury to bladder and rectum.