Introduction
Cervical adenocarcinoma is seen to be accounting to about 10–20% of invasive carcinoma cervix. These carcinomas have poor radiosensitivity and chemosensitivity.1, 2 The Papillary serous carcinoma of the uterine cervix (PSCC) is a very rare variant of adenocarcinoma of cervix. What makes it so unique, is that it histologically resembles the same tumour occurring very commonly in sites namely, the ovary, fallopian tube, endometrium, and also peritoneum.3
The Fallopian tube carcinoma was assumed to be a rare occurance,thereby an emphasis of fallopian tube malignancies has been seen of late. This lead to the development of a new concept of recognising serous carcinomas of ovarian type frequently involved the fallopian tube fimbria. The fallopian tube epithelium was found to be the origin of major high grade ovarian serous carcinomas. This new concept has now drawn attention for ascertaining the role of fallopian tubes in gynaecological malignancies and, this can be achieved when the entire fallopian tube will be subjected for histologically analysis.4, 5
Primary fallopian tube carcinomas account to about 0.1-1.8% of all genital malignancies, and it is very difficult to diagnose preoperatively, because of its non-specific symptomatology.6
Here, is a case with similar situation being presented at our hospital.
Case Report
A 58 years old woman, was apparently normal 2 months back, when she started to notice pain abdomen which was dull aching, intermittent in the beginning and then gradually became continuous type of pain. No aggravating or relieving factors, no radiating pain as well.
She gave history of white discharge per vagina since 15 days, on and off, moderate in amount, serous in consistency, not associated with itching and non foul smelling, changing one cloth per day. History of post-menopausal spotting Per vagina – 2 episodes in a span of 15 days was present. History of burning micturition, increased frequency of micturition and urge incontinence since 15 days.
On patient being received at RLJ Hospital, was found to be well oriented to time, place and person, moderately built and nourished. Pulse was 82 bpm, regular, good volume, regularly regular, no radioradial or radiofemoral delay and Blood pressure: 110/70 mm Hg, right arm,supine, lateral position; temp : 99 degree F. Systemic examination was examined to be normal.
On per speculum examination, -Cervix appeared hypertrophied, posteriorly cervix flushed into the vagina, 1cmx1 cm ulcerative lesion over cervix present at 9 o’clock position1% acetic acid applied , no distinctive acetowhite areas present, Bleeds on touch.cervical punch biopsy was taken, profuse mucoid fluid coming out through the OS, not foul smelling. Per vagina: Uterus was 6 weeks size, retroverted, mobility restricted, profuse mucoid fluid coming out through the OS, not foul smelling Bilateral fornices free non tender. fluid was sent for cytology
The patient came with an outside PAP smear report and ultrasound. The PAP showed LSIL(Low-grade squamous intraepithelial lesion) and the ultrasound performed showed uterus small and atrophic. Hypoechoic lesion measuring 5.1x3.9 noted in the left adnexa. Suggestive of Haemorrhagic cyst of left ovary suggested CECT/MRI pelvis for further evaluation. She went on to get a MRI which later on reported as MRI Pelvis: uterus- fluid in endometrial cavity with fluid levels measuring 6x3 cm. cervix- multiple nebothian cysts in cervix measuring 16x12 mm. no obvious mass in cervix. Impression: features suggestive of probably hematometra secondarty to cervical stenosis. For further evaluation endometrial biopsy was taken and the section studied showed occasional fragmented glands in the background of haemorrhage and fibrinous exudate.
Cervical punch biopsy
Section studied shows fragment of ectocervical lining and endocervical glands with mild inflammatory cells infiltrating the fibrocollagenous tissue. No dysplasia/malignancy noted. The Intrauterine fluid taken showed many neutrophils, and a few benign epithelial cells and degenerated cells. Background shows proteinaceous debris. Negative for malignant cells.
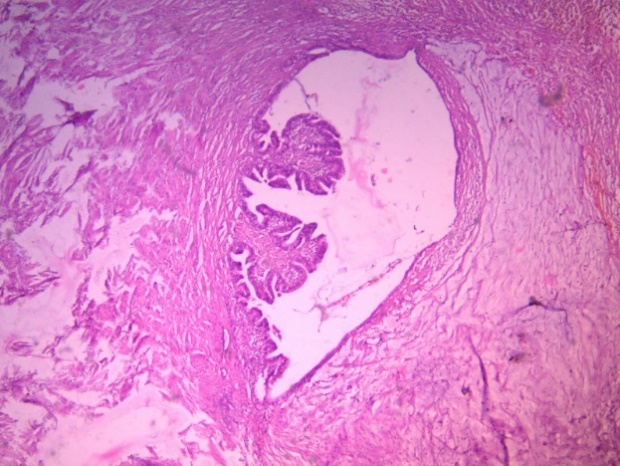
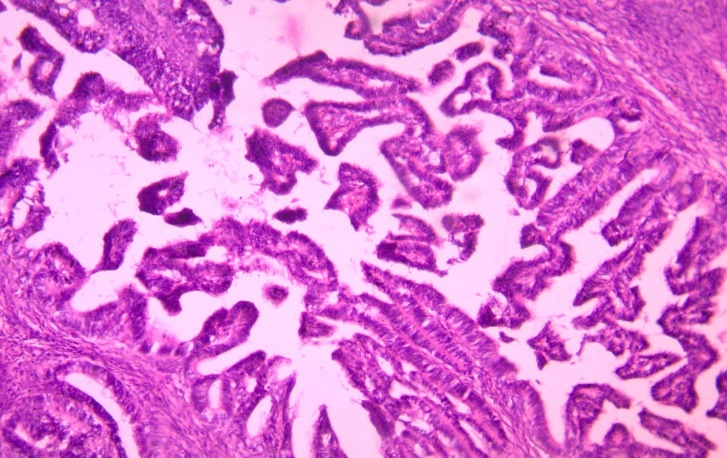
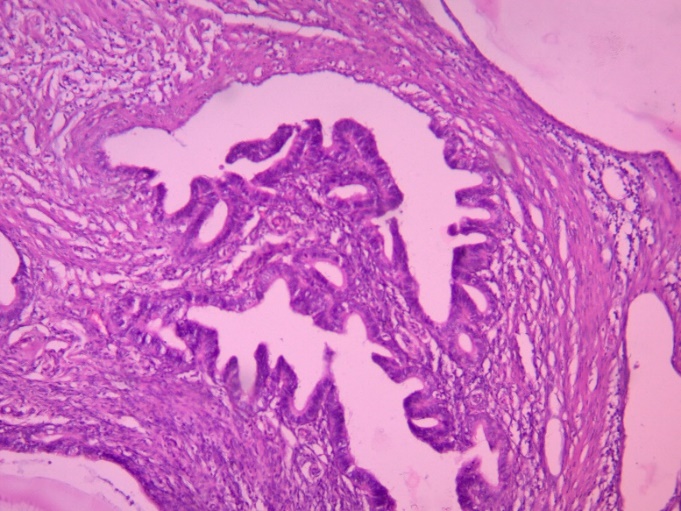
After routine investigations and preoperative work up, patient was taken up for Total Abdominal Hysterectomy with Bilateral Salphingoophorectomy with an indication of CIN II on 14/5/19. On table, there was no complications, uterus was 6 weeks size, bilateral tubes and ovaries appeared normal. Post operative period was uneventful. The Histopathology report showed section studied from cervix – reveals normal ectocervical lining epithelium with endocervical area showing tumor composed of malignant glands arranged in tubular and papillary configuration with round to oval tumour cells with high N:C ratio, vasicular nuclei, nuclear crowdy, presence of mitotic figures and ciliated lining. The glands are seen infiltrating the underlying stroma. No lymphovascular perineural invasion seen. Features suggest of serous papillary adenocarcinoma – cervix. Section studied from left fallopian tube shows tumor with similar morphology described above s/o serous papillary adenocarcinoma – left fallopian tube.
Patient has now been started with radiotherapy and chemotherapy with weekly Carboplatin 150mg.
Discussion
A proportion of 18.5% to 27% of carcinoma cervix are of adenocarcinoma type. Intraepithelial or invasive squamous neoplasia appears in 30% to 50% of cervical adenocarcinomas. A squamous intraepithelial lesion can be detected when the ectocervix is visualized colposcopically and it is also witnessed that the coexistent adenocarcinoma is frequently greater in the cervical canal.7 In about 70% of adenocarcinoma of cervix, Endocervical type is discovered to be very common.1, 7 On the contrary, Papillary serous carcinoma of the uterine cervix (PSCC) is found to be one of the rarely encountered subtype and also very recently been described subtypes of endocervical adenocarcinoma.1, 8, 9 Of late, only 46 cases of PSCC have been found to be reported in the literature and merely one large series consisting 17 cases have been documented which has been brought to us by study conductd by Zhou et al.2, 3 PSCC is an aggressive neoplasm and need for distinguishing it histologically from other papillary carcinomas of cervix which have better prognosis like villoglandular papillary adenocarcinomas should be given atmost importance. On visualising the tumor microscopically, it is seens that it has a papillary or glandular pattern, to start with, the tumour cells display hyperchromatic nuclei, with generally more than ten mitotic figures and infrequent psammoma bodies. This microscopic picture was insync to the microscopic picture documented in our case as well.
There is bimodal age distribution of PSCC noted, with one peak witnessed before the age of 40 years and the second peak seen after the age of 54 years.3, 9 The patient that presented to us was diagnosed at age 58, which verifies the typical age distribution.
The pelvic and periaortic lymph nodes are the most common sites for metastases following them are lymph nodes of the cervix, the peritoneum, the lung, the liver, and skin.3 However, in our case, there was no ovarian, peritoneal, or uterine masses found.
For stage I and II of PSCC, the treatment strategies available includes surgery alone, radiotherapy alone10 or primary surgical therapy followed by postoperative radiotherapy.11 Initially, a lack of response of PSCC to chemotherapy with paclitaxel and carboplatin had been reported3 but quite recently, a study by Ueda et al. testified an excellent response of stage IVb PSCC to a primary combination neoadjuvant chemotherapy with paclitaxel and carboplatin before the debulking surgery.5 Taking this in to account, after contemplating, Our patient who had undergone total abdominal hysterectomy and bilateral salpingo-oophorectomy was to be followed up by a combination chemotherapy and radiotherapy.
Conclusion
The adenocarcinoma of the fallopian tube and uterine cervix coexistence, in the lack of relevant lesion on the body of the uterus, is a very unusual condition. This leads to reasoning, to whether the coexistence of these two tumors is incidental or metastatic or either.12 In our case, this rare condition presented to us where there was no contiguous disease - the uterine body, right fallopian tube and the ectocervix was free from lesion more like skipped lesions. An attempt was made from our side to recognise this relationship, and we come to a conclusion that it was found to be incidental. The idea of bilateral Salphingoophorectomy done for this patient helped in the early detection of fallopian tube carcinoma.