Introduction
Pregnancy and childbirth are a significant milestone in the life of a woman but sometimes these physiological events are complicated by some unique disorders that lead to significant morbidity and even mortality. Preeclampsia / eclampsia along with haemorrhage and sepsis form the deadly triad of maternal mortality; accounting for 63000 direct maternal deaths worldwide(13% of all direct causes) with more than 4 million cases per year.1
Preeclampsia is defined as new onset hypertension greater than equal to 140/90 mm Hg after 20 weeks of pregnancy with proteinuria greater than equal to 300 mg /24 hours or greater than equal to 1+ dipstick (NHBPEP)2 (ISSHP).3 It complicates 2-8% of all pregnancies. As it is an important cause of both foetal and maternal morbidity and mortality early diagnosis and intensive management is of utmost necessity. If preeclampsia can be diagnosed at an incipient stage intensive obstetric care can be utilised more effectively in patients who are at greater risk.
Though the exact aetiology and pathogenesis of preeclampsia remains unclear even today, recent understanding of the disease process has identified a two stage model, where the first stage is poor placentation and the second stage of placental oxidative stress and inflammation.4 This understanding has led to the development of numerous screening tests for this disorder.
Alpha-fetoprotein (AFP) is the most abundant plasma protein found in human foetus. It is produced by foetal liver and GI tract. In preeclampsia there is poor placentation due to trophoblastic dysfunction. This causes increased leakage of this foetal protein into maternal blood leading to its increased level in maternal serum. Beta- hCG and Inhibin -A are secreted from the foetal syncytiotrophoblasts. In preeclampsia due to dysfunction of these trophoblastic cells there is increased level of these proteins in maternal serum.5, 2, 3
Aim of this present study is to analyse the potential clinical use of these biochemical parameters (serum beta hCG, AFP, Inhibin -A) for the purpose of prediction of preeclampsia.
Aims and Objectives
Application of maternal second trimester serum parameters like AFP, beta -hCG, Inhibin -A to predict preeclampsia in apparently healthy pregnant patients.
Materials and Methods
Sample size
Two hundred (200) patients had been investigated during the process of the study and were followed up till delivery.
Study technique
Any pregnant woman attending the antenatal clinic (OPD) at 12-14 weeks of pregnancy satisfying the inclusion criteria of this study had been examined thoroughly and her history was taken properly. Data was collected from all eligible candidates with informed consent. Assessment of serum parameters i.e. β-hCG, AFP, Inhibin-A were done between 12 and 16 weeks of gestation. All the pregnant women in the study population were followed up till their delivery. The number of women in the study population who developed preeclampsia were seen and sensitivity, specificity and predictive values of each serum parameter was calculated.
Data analysis
Categorical variables are expressed as Number of patients and percentage of patients.
Presence and absence of Preeclampsia is compared across different categorical variables using Pearson’s Chi Square test for Independence of Attributes.
Continuous variables are expressed as Mean ± Standard Deviation and compared across the 2 groups (Developed and Not developed Preeclampsia) using unpaired t test.
ROC curve analysis is done to establish the cut offs for MOM msAFP(ng/mL)(12-16 weeks), MOM msβ-hCG(IU/mL)(12-16 weeks), MOM msInhibin-A(pg/mL) (12-16 weeks).
Sensitivity, specificity, Positive Predictive Value, Negative Predictive Value and Diagnostic Accuracy was obtained for the cut offs.
The statistical software SPSS version 20 has been used for the analysis.
An alpha level of 5% has been taken, i.e. if any p value is less than 0.05 it has been considered as significant.
Results and Analysis
The present study is a hospital OPD based prospective study commencing from 1st July 2013 to 30th June 2014. During this time 200 randomly selected (fulfilling inclusion and exclusion criteria) antenatal patients were taken and serum (β-hCG, AFP, inhibin-A) tests were done at appropriate times. All the women were followed till delivery for development of preeclampsia (defined as: BP≥140/90 mm Hg and Uristix protein≥1+).
Categorical variables are expressed as Number and percentage of patients.
Presence and absence of Preeclampsia is compared across different categorical variables using Pearson’s Chi Square test for Independence of Attributes.
Continuous variables are expressed as Mean ± Standard Deviation and compared across the 2 groups (Developed and Not developed Preeclampsia) using unpaired t test.
ROC curve analysis is done to establish the cut offs for MOM msAFP(ng/mL)(12-16 weeks), MOM msβ-hCG(IU/mL)(12-16 weeks), MOM msInhibin-A(pg/mL) (12-16 weeks).
Table 2
Frequency distribution of age in the study population
|
Age( years) |
Frequency |
Percent |
|
<20 |
52 |
26 |
|
21-25 |
90 |
45 |
|
26-30 |
40 |
20 |
|
31-35 |
17 |
8.5 |
|
36-40 |
1 |
0.5 |
|
Total |
200 |
100 |
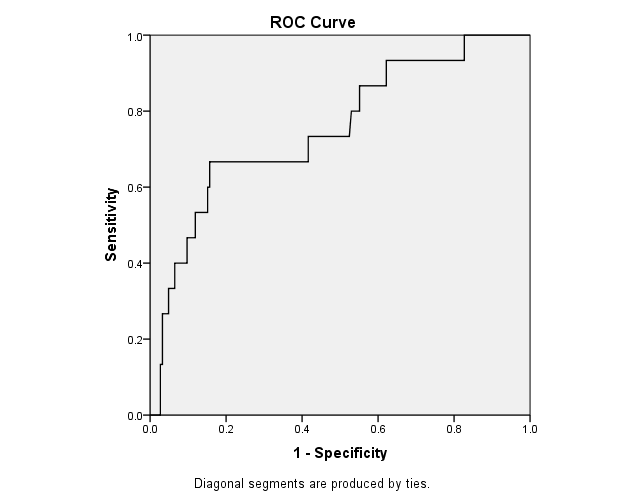
Graph showing the ROC curve of MOM MS AFP (12-16 weeks). Cut off value of MOM MS AFP that can predict preeclampsia was calculated from the curve.
Cut off MOM MS AFP= 2.158
AUC of the ROC curve= 0.753
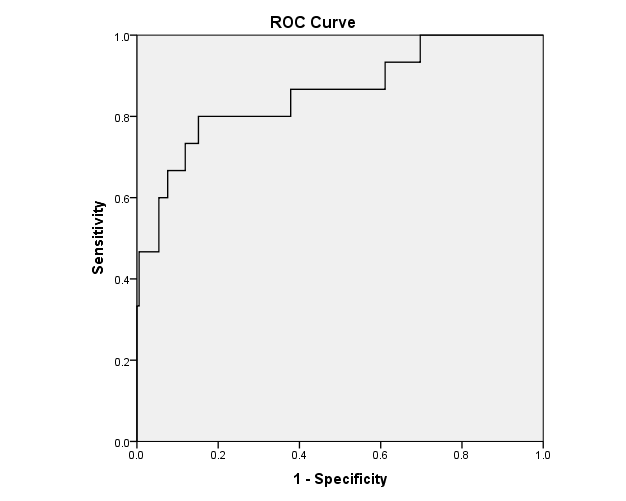
Graph showing the ROC curve of MOM MS β-hCG (12-16 weeks). Cut off value of MOM MS AFP that can predict preeclampsia was calculated from the curve.
Cut off MOM MS hCG=2.499 AUC of the ROC curve=0.857
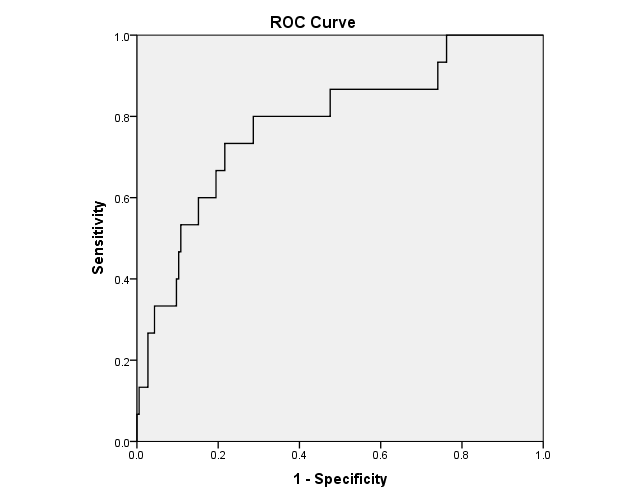
Graph showing the ROC curve of MOM MS inhibin-A (12-16 weeks). Cut off value of MOM MS inhibin-A that can predict preeclampsia was calculated from the curve.
Cut off MOM MS inhibin-= 2.454
AUC of the ROC curve= 0.784
In the next section each of these parameters individually and in combination are evaluated for their sensitivity, specificity and predictive values as predictor of preeclampsia.
Table 3
Comparison of MS AFP (12-16 weeks) and development of preeclampsia
|
Cut off MOM: 2.158 |
MOM MS AFP |
Total |
||
|
Normal |
High |
|||
|
Developed preeclampsia |
No |
156 (96.89%) |
29 (74.36%) |
185 |
|
Yes |
5 (3.11%) |
10 (25.64%) |
15 |
|
|
Total |
161 |
39 |
200 |
|
Table 3 showing comparison of MOM MS AFP with development of preeclampsia. Among the 39 subjects whose MOM AFP was high i.e. above cut off 10 developed preeclampsia, 5 subjects among 161 developed preeclampsia yet their MOM AFP level was normal.
Table 4
Comparison of msβ-hCG (12-16 weeks) and development of preeclampsia
|
Cut off MOM: 2.499 |
MOM msβ-hCG |
Total |
||
|
Normal |
High |
|||
|
Developed preeclampsia |
No |
157 (98.13%) |
28 (70.00%) |
185 |
|
Yes |
3 (1.87%) |
12 (30.00%) |
15 |
|
|
Total |
160 |
40 |
200 |
|
Table 4 showing comparison of MOM MS β-hCG with development of preeclampsia. Among the 40 subjects whose MOM β-hCG was high i.e. above cut off 12 developed preeclampsia, 3 subjects among 160 developed preeclampsia yet their MOM β-hCG level was normal.
Table 5
Comparison of msinhibin-A (12-16 weeks) with development of preeclampsia
|
Cut off MOM: 2.454 |
MOM ms Inhibin A |
Total |
||
|
Normal |
High |
|||
|
Developed preeclampsia |
No |
145 (97.32%) |
40 (78.43%) |
185 |
|
Yes |
4 (2.68%) |
11 (21.57%) |
15 |
|
|
Total |
149 |
51 |
200 |
|
Table 5 showing comparison of MOM MS inhibin-A with development of preeclampsia. Among the 51 subjects whose MOM inhibin-A was high i.e. above cut off 11 developed preeclampsia, 4 subjects among 149 developed preeclampsia yet their MOM inhibin-A level was normal.
Comparison of mean of continuous variables of different tests:
Figure 4 showing comparison of mean of MS AFP of those developing and not developing preeclampsia. The difference was significant (2.05 vs 1.48; p=0.001).
Figure 5 showing comparison of mean of MS β-hCG of those developing and not developing preeclampsia. The difference was significant (2.73 vs 1.59; p<0.001)
Figure 6 showing comparison of mean of MS inhibin-A of those developing and not developing preeclampsia. The difference was significant (2.48 vs 1.70; p<0.001).
Discussion
Preeclampsia is a unique pregnancy specific hypertensive disorder with a variety of manifestations involving various organ systems of the body. It is a major cause of feto-maternal morbidity and mortality worldwide.1, 4 Pathogenesis of preeclampsia has remained a mystery for investigators for decades. But present understanding of the disorder has unveiled that defective trophoblastic endovascular remodelling of the maternal spiral arteries followed by oxidative stress of the placenta with endothelial activation6, 7 and generalised inflammatory reaction of the mother is the central theme of this disorder. Immune maladaptation remains the underlying cause. Basic theme of the various predictive tests for preeclampsia, has been to identify a specific pathogenic process related to preeclampsia and detect it sufficiently early in the asymptomatic stage to identify those who will subsequently develop the syndrome of preeclampsia. Although a WHO meta-analysis by Conde-Agudelo and associates in 2004 concluded that there is no suitable screening test with reasonable sensitivity and specificity that can predict preeclampsia; but various authors have also employed a wide variety of tests with variable predictive value for the said purpose. Our present study was intended at preeclampsia prediction by identifying the pathological processes involved in its pathogenesis:
Table 0
|
Test name |
Pathogenic basis of the test |
|
1. Maternal serum β-hCG, AFP, Inhibin-A |
Increased secretion by the hyperplastic syncytiotrophoblasts (STB). |
The present study was an OPD based prospective study conducted from 1st July 2013 to 30th June 2014, which included 200 randomly selected antenatal patients 12-14 weeks of pregnant that met the inclusion criteria. A thorough history was taken from all these patients with informed consent and basic investigations were performed. Serum parameters β-hCG, AFP, Inhibin-A were done between 12 and 16 weeks of gestation. All the patients were followed up till delivery for the development of preeclampsia (defined as BP ≥140/90 mm Hg and Uristix protein ≥1+). The different characteristics of the patient population were analysed to find a significant association with development of preeclampsia. Also the value of the predictive tests were determined in terms of sensitivity, specificity, PPV and NPV for the purpose of prediction of preeclampsia. Among the various demographic and basic clinical and laboratory parameters BMI and booking uristix protein had significant association with development of preeclampsia. For BMI, higher it was higher was the risk of developing preeclampsia (mean 23.91 vs 21.93 for preeclampsia and normal pregnancy respectively; p=0.002). This is also consistent with studies by O’ Brien et aland Cedergren et al. For proteinuria, more subjects with trace proteinuria developed preeclampsia than non-proteinuric subjects (18.6% vs 4.46%; p=0.002). Regarding the screening tests, first the cut-off values for comparison were set by constructing ROC (receiver operating characteristic) curves for each test and then they were compared for determination of predictive values of each test, as there is no standardized cut off for these tests.
Serum parameters done between 12-16 weeks of pregnancy yielded the following data: MS AFP was found raised above the cut off (cut off 2.158 MOM) in 39 subjects; of them 10 subjects developed preeclampsia. The sensitivity, specificity, PPV and NPV of AFP for prediction of preeclampsia were 66.67%, 84.32%, 25.64% and 96.89%. MS β-hCG was found raised above cut off (cut off 2.499 MOM) in 40 subjects; of them 12 subjects developed preeclampsia. The sensitivity, specificity, PPV and NPV of β-hCG for prediction of preeclampsia were 80.00%, 84.86%, 30.00% and 98.13%. MS inhibin-A was found raised above cut off (cut off 2.454 MOM) in 51 cases among them 11 subjects developed preeclampsia. The sensitivity, specificity, PPV and NPV of inhibin-A for prediction of preeclampsia were 73.33%, 78.38%, 21.57% and 97.32%. comparison of mean of MOM of these parameters showed significant association with development of preeclampsia (2.05 vs 1.48 for AFP p=0.001, 2.73 vs 1.59 for β-hCG p<0.001, 2.48 vs 1.7 for inhibin-A p<0.001). Study by Aquilina et al.8 used β-hCG and inhibin-A (cut off >2.0 MOM) and found sensitivity of Inhibin-A to be greater than hCG (48.6% vs 37.4%) fixing specificity at 90% (p<0.05) for preeclampsia prediction. Yaron et al.9 found significant association with preeclampsia and other adverse pregnancy outcomes when β-hCG and AFP were >2.5 MOM (p<0.001). Gravett et al.10 (using β-hCG>5.0 MOM, AFP>2.5 MOM), Gonen et al.11 (using β-hCG>3.0 MOM, AFP>2.5 MOM), Cuckle et al.12 (using inhibin-A>2.01 MOM), Duric et al.13 (using β-hCG>2.0 MOM, AFP>2.02 MOM) and Wald et al14 (using inhibin-A>1.7 MOM, β-hCG>2.1 MOM) all found significant association with preeclampsia development. Luckas et al.7 studied the mean MOMs and found raised hCG MOM (1.52 vs 1.10; p=0.03) to be 79% sensitive and 54% specific for preeclampsia. Lack of standard cut off MOM for these parameters limits proper comparison between these studies. Negative studies by Davidson et al15 and Lambert-Messerlian16 found no association between these parameters and preeclampsia. Our study found significant association with all the serum parameters namely β-hCG, AFP and inhibin-A and preeclampsia, consistent with previous studies.