Introduction
Intestinal obstruction (IO) in pregnancy is rare at 1 in 25001 to 1 in 167092 deliveries with an incidence of 0.001% to 0.003%. Although uncommon, IO in pregnancy carries significant maternal (6%) and fetal (26%) mortality.3 Preterm delivery occurs in ∼45% of the cases.4 Adhesions are the commonest cause of IO in pregnancy and account for more than half the causes found at laparotomy. Other causes include volvulus (23%), intussusception (5%), hernia (3%), carcinoma (1%), appendicitis (1%), and idiopathic “ileus” (8%).3 The incidence and complication rates increase with gestational age, particularly in the third trimester The most common presenting symptoms are abdominal pain (88%), vomiting (67%), examination findings of tenderness (49%) and distension (28%).5 Diagnosis of SBO can be difficult to make as symptoms are often attributed mistakenly to the pregnancy and there can be a reluctance to request plain films owing to the risks of ionising radiation. Both of these factors can lead to a delay in diagnosis and initiating treatment. Previous literature reviews have placed great importance on aggressive management with prompt laparotomy once a diagnosis of SBO has been made, with no role for conservative treatment, part of this argument being that the aetiology of the SBO cannot be determined until a laparotomy has been performed.3, 6 There is no agreed treatment strategy for patients presenting with SBO in pregnancy. Optimal management depends on a number of factors including aetiology of the obstruction and gestational age of the fetus. Perinatal death from hypoxia secondary to maternal hypovolaemia, sepsis, and peritonitis has been reported.
Case Report
A 30-year-old, primigravida, at 33weeks 4 days of gestation presented to the emergency obstetrics department of Swaroop Rani Nehru Hospital, Prayagraj, Uttar Pradesh, India with a 2-day history of diffuse abdominal pain, distension and obstipation. The patient also reported two episodes of bilious vomiting. She had no history of fever, any urinary symptoms and her pregnancy had been uneventful till date. Past surgical history included a laparotomy for small bowel volvulus 4 years back. There was no significant medical history.
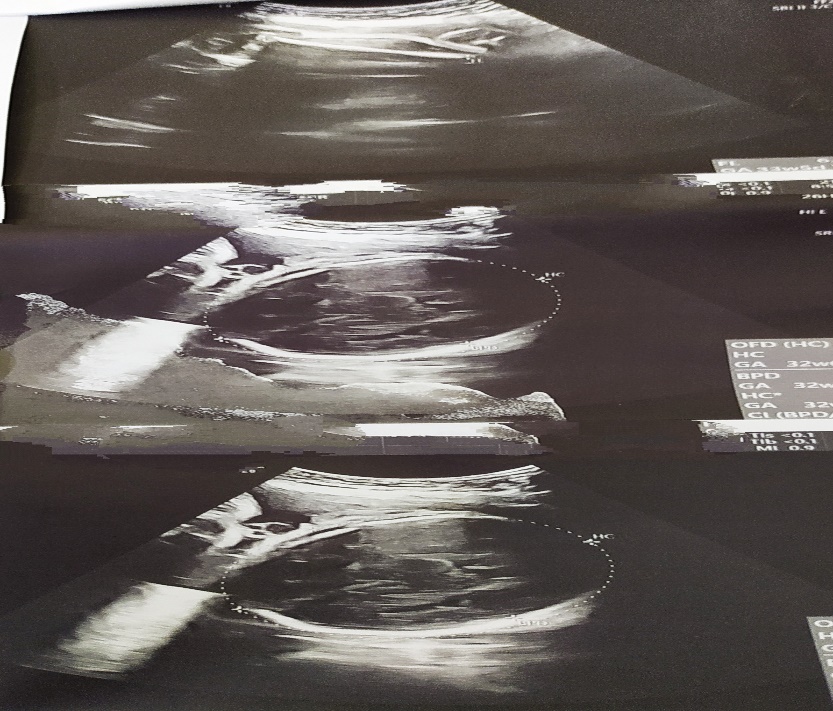
On examination, she was afebrile with normal blood pressure and pulse rate. Abdominal examination revealed epigastric tenderness and abdominal distention, with no signs of guarding or rigidity. The uterus was soft and there were no palpable contractions. Her fetal heart was regular. Laboratory studies showed a Total leucocyte count of 19.56 × 109cells/l, C-Reactive Protein (CRP) was 69 mg/l and haemoglobin was 7.9 g/dl. Her liver function test and kidney function test were within normal limits. The patient underwent a trans-abdominal ultrasound scan showing a single live intrauterine fetus of 33weeks 1 day in longitudinal lie and cephalic presentation with normal placenta, AFI = 9cm and effective fetal birth weight of 2.5kg with dilated small bowel loops.
Urgent surgery consultation was done and a provisional diagnosis of possible SBO was made. She was managed conservatively and commenced on IV fluids, antiemetics, antispasmodics, antibiotics and nasogastric tube was inserted which gave symptomatic relief. Fetal lung maturation was induced with dexamethasone. Over next 48 hours, her symptoms worsened with increasing abdominal pain, distention, bilious vomiting and high volumes of nasogastric aspirate. Fetal bradycardia was also noted. The decision of emergency caesarean section was taken and a 2.5kg healthy female baby was delivered. Surgical opinion was sought intraoperatively.
On examining the bowel, there were several small bowel loops adherent to one another and adhesiolysis was done. High grade SBO approximately 12–15cm from the ileocaecal valve with proximal small bowel dilatation and collapsed distal ileum was. Signs of impending perforation were demonstrated by multiple serosal tears in conjunction with areas of necrosis. Segmental resection and anastomosis with appendicectomy was done. One unit of packed RBC was transfused per-operatively. Postoperatively she recovered well and the mother and the baby were discharged on 10th day in satisfactory condition.
Discussion
Diagnosis of SBO can be difficult to make as symptoms are often attributed mistakenly to pregnancy and there can be a reluctance to request plain films owing to the risks of ionising radiation. Both of these factors can lead to a delay in diagnosis and initiating treatment. Clinical suspicion is vital and joint management between surgeons and obstetricians is crucial. In 2013 the American College of Radiology concluded that present data have not documented conclusively any deleterious effects of MRI exposure on the developing fetus, with no special considerations being recommended for any trimester of pregnancy. This makes it a useful tool for imaging the small bowel and diagnosing SBO in pregnancy.7
In 2015 review of literature,8 overall rate of fetal loss was 17% (n=8) and the maternal mortality rate was 2% (n=1). These figures have improved since the last review in 1992, where fetal loss occurred in 26% of cases and maternal mortality was 6%.9 As with previous reviews, adhesions were the most common cause of SBO (n=23, 50%). Twenty-one patients (91%) with adhesional SBO were managed surgically, including sixteen (76%) who failed conservative treatment. Three of the fetal deaths occurred in patients with adhesional SBO. There were no fetal deaths in the first trimester, two in the second trimester and one in the third trimester. All three cases of fetal loss were from the same case series10 and in all three cases, the patients were managed surgically. Two of the patients were operated on 13 days after the onset of symptoms and the other patient after 6 days. Two patients with adhesional SBO were managed conservatively.10, 11 Meyerson et al. managed a patient with adhesional SBO conservatively from 31 weeks’ gestation up until delivery at 36 weeks.10 Phillips et al. managed a patient with SBO conservatively at 26 weeks’ gestation, resolving the acute episode.11 The patient continued to have episodes of incomplete obstruction throughout pregnancy and was managed with instigation of an elemental diet until she delivered at 38 weeks. In both cases, there was no fetal loss or maternal mortality.
Since the last literature review in 1992,9 CT and MRI have become more readily available and have been employed in the acute setting to diagnose SBO in pregnancy. In the 2015 review, six patients (13%) had urgent CT and five separate patients (11%) had urgent MRI. MRI is capable of multiplanar imaging, excellent soft tissue contrast and avoids the risks of ionising radiation. This makes it a useful tool for imaging the small bowel and diagnosing SBO in pregnancy.12
The initial treatment consists of nasogastric aspiration with aggressive IV fluids to correct electrolyte disturbances. Failure of conservative treatment are indications for early surgery as persistence will contribute to an increase in maternal and fetal mortality and morbidity. Maternal nutritional deficiencies can occur if the patient is kept nil per oral (NPO) for a protracted period. Surgery should be performed via a midline incision to allow adequate exposure and complete exploration of abdomen. The entire bowel must be examined for other areas of obstruction and viability. Segmental resection with or without anastomosis may be necessary in the presence of gangrenous bowel.
There is no agreed treatment strategy for patients presenting with SBO in pregnancy. Previous literature reviews have placed great importance on aggressive management with prompt laparotomy once a diagnosis of SBO has been made, with no role for conservative treatment, part of this argument being that the aetiology of the SBO cannot be determined until a laparotomy has been performed. Optimal management depends on a number of factors including aetiology of the obstruction and gestational age of the fetus. While in agreement with previous literature reviews regarding the need for prompt laparotomy in most cases of SBO, we recommend that patients with confirmed adhesional obstruction may be managed conservatively in the first instance but with a low threshold for progressing to laparotomy.
Conclusion
SBO in pregnancy is most commonly due to adhesions from previous abdominal surgery, and carries significant risks to both mother and fetus. Cases should be managed on an individual basis with a multidisciplinary team approach. A high degree of suspicion is crucial, especially in patients with previous abdominal surgery. The high morbidity and mortality rates meant that radiological investigations and surgery should not be delayed. An additional learning point from this case would be that in an obstetric patient without any surgical history who presents with abdominal pain, one should always consider rarer surgical causes other than merely obstetric or gynaecological causes of pain.
Due to low case numbers and the emergency nature of the diagnosis, prospective studies would be impractical to determine optimum timing for emergency surgery. Data however collected retrospectively, would provide other valuable information such as length of hospital stay, average gestational of delivery on conservative management, surgical site infection rates and findings of incidental or causative pathology in specimens.