Introduction
Acute colonic pseudo-obstruction syndrome, a rare condition with serious morbid complication that occurs in postoperative course of obstetric and gynaecological patients, difficult to diagnose. It is characterised by massive dilatation of caecum and colon upto splenic flexure without any mechanical obstruction. It is reported most commonly in elderly age group with co-morbidities. Caesarean section is considered as one of the predisposing factor for this condition in reproductive age group. Early identification and prompt treatment reduces the risk of caecal perforation. Here we report a case of anterior caecal wall necrosis with perforation after a caesarean section requiring emergency laprotomy.
Case Report
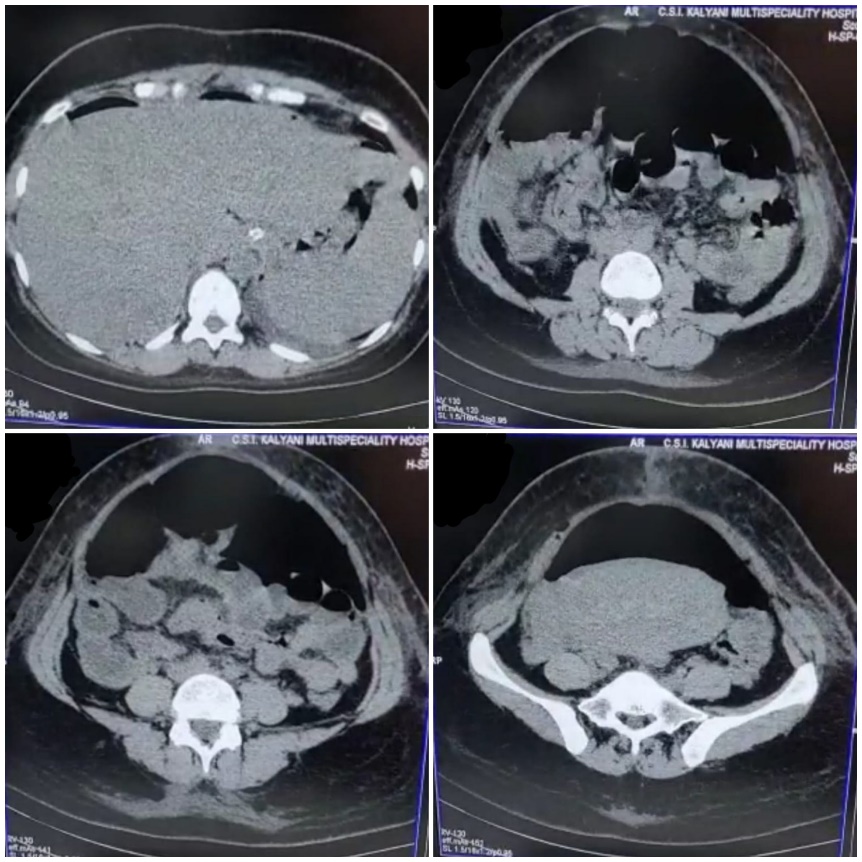
A 28 years old, low risk primigravida of gestational age 39 weeks 5 days admitted at our hospital for safe confinement. Labour induced with cerviprime gel and later she underwent emergency LSCS in view of non progression of labour. Intraoperative period was uneventful and estimated blood loss was approximately 500ml. Immediate postoperative period, patient is hemodynamically stable.12hours later bowel sounds checked, oral fluids started. On the same day, patient developed mild gaseous distention. On POD2 abdomen distention increased and patient developed obstipation and shoulder tip pain. Bowel sounds became sluggish. Serum electrolytes were in the lower limit of normal. X-ray abdomen erect suggestive of wide spread colonic dilatation with no free air. Paralytic ileus is suspected and proceeded for conservative management. Patient kept on NPO, continuous ryle’s tube aspiration and started on higher iv antibiotics. Despite of conservative management patient continue to have symptoms. CECT abdomen and pelvis suggestive of diffuse pneumoperitoneum with dilated small bowel loops seen along the centre part of abdomen suspected subacute bowel obstruction as shown in Figure 1, hence patient taken up for emergency laparotomy on POD 4.
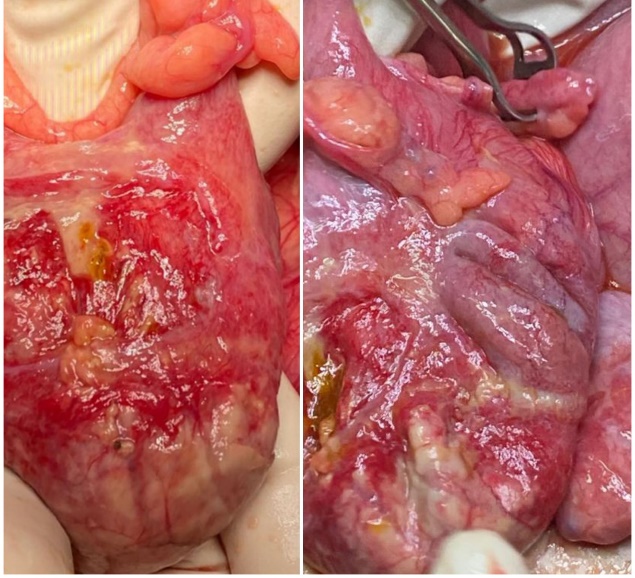
Intraoperative finding are anterior caecal wall gangrene with perforation with dilated and congested small bowel loops shown in Figure 2. No evidence of mechanical obstruction.
Excision of gangrenous part done followed by distal stump closure and covering loop ileostomy done. Postoperatively patient recovered well and ileostomy closure with ileocolic anastomosis done after 3 months.
Discussion
The main finding in our case report is post caesarean patient developing functional bowel obstruction in the early post operative period. There are two types of functional bowel obstruction known in obstetrics:
Paralytic ileus occurs from prolonged hypomotility of GI tract secondary to inflammation of intestinal smooth muscles. Acute colonic pseudo-obstruction syndrome which is reported in our case is a rare acquired complication associated with high morbidity and mortality rate where the exact pathogenesis is not clearly known. It is characterised by abnormalities affecting the involuntary rhythmic muscular contractions within the colon due to imbalance between the sympathetic and parasympathetic nervous system, i.e. increased sympathetic and decreased sacral parasympathetic activity. Moreover in postpartum period there is a decline in serum estrogen level which further decreases the parasympathetic tone leading to atonic distal colon and functional proximal colon obstruction.1, 2 Some possible risk factors for this condition in obstetrics includes prolonged labour, maternal fatigue, electrolyte imbalance, regional anaesthesia, operative deliveries.3, 4 In our case the possible risk factors are caesarean section and regional anaesthesia. Colonic dilatation causes tension on wall, leading to ischemia and perforation. Caecum having the largest resting diameter is more prone for easy dilatation (Law of Laplace) and hence for necrosis and perforation. A caecal diameter of 9cm and beyond increases the risk of colonic perforation. Caecal diameter is the principal prognostic factor for deciding the management and the prognosis of the patient. First line of investigation is X-ray abdomen in erect posture but the imaging modality of choice is CT abdomen which differentiates this condition from mechanical bowel obstruction and gives the idea about caecal dilatation accurately. Initial management when there is no evidence of perforation includes conservative management by keeping the patient nil per orally, Ryle’s tube aspiration, correction of electrolyte imbalances and strict ambulation may relieve ileus. If colonic dilatation is more than 9–10 cm, pharmacological therapy with neostigmine injection or endoscopic colonic decompression with a large flatus tube can be tried.5 Immediate response by passage of flatus and sustained response by decrease in abdominal distension can be noted.6 The success rate is found to be 77 to 96%.7 Other medications like erythromycin and metoclopramide also can be tried. In our case, since our patient went in for perforation laparotomy was proceeded.
Conclusion
Every obstetrician should be aware of acute colonic pseudo-obstruction syndrome which can occur in caesarean section but mechanical obstruction should always be ruled out by investigation. Clinical suspicion, careful follow up and early diagnosis of this syndrome will help us to decrease the morbidity of the patient.