Introduction
Endometrial polyps are outpouching of endometrial glands and stroma arising from the endometrial cavity of the uterus. They are of different sizes. They may range from few millimeters to several centimeters in diameter. The polyp may occur as a solitary lesion or multiple lesions occupying the entire endometrial cavity.1 Endometrial polyps contribute to infertility and recurrent pregnancy loss through different mechanisms. They are reported to interfere with fertility by obstructing sperm transport, embryo implantation, or inflammation of uterus. They are known to increase the production of inhibitory factors such as glycodelin in uterine fluid.2 Before implantation endometrium should be made receptive for the embryo which requires a detailed process in a time- and location-specific manner.3 Though various pathologies like submucous fibroids, polyps, adhesions, and endometritis interfere with fertility, endometrial polyps are the common intrauterine pathology and are benign.4 Polyps are mostly asymptomatic. They are accidentally discovered during transvaginal ultrasound for evaluation of female infertility.5 Sometimes they cause abnormal uterine bleeding.
Endometrial polyps in general population are reported to be 10%.6 Studies have shown high prevalence of endometrial polyps in infertile patients ranging from 6% to 32%.7, 8 Endometrial polyps may account for a causative relationship between endometrial polyps and infertility. Pregnancy rates ranging from 23% to 65% have been reported after polypectomy in infertile patients.9, 10, 11 Endometrial polyps are diagnosed by transvaginal ultrasound with 86% sensitivity, 94% specificity, 91% positive predictive value and 90% negative predictive value.12 Diagnostic hysteroscopy is an effective tool in confirming the size and nature of the polyps with a sensitivity of 58% to 99% and specificity of 87 to 100% in different studies. Hysteroscopy with biopsy is considered to be the gold standard in the diagnosis of endometrial polyps.11 Removals of endometrial polyps prior to IUI or embryo transfer in ART patients have shown significant improvement in cumulative pregnancy rates.
The aim of our study is to find the clinical pregnancy rates after endometrial polypectomy in patients undergoing Intracytoplasmic sperm injection cycles and also to study the different locations of endometrial polyps in the uterine cavity and their relation with pregnancy rates.
Materials and Methods
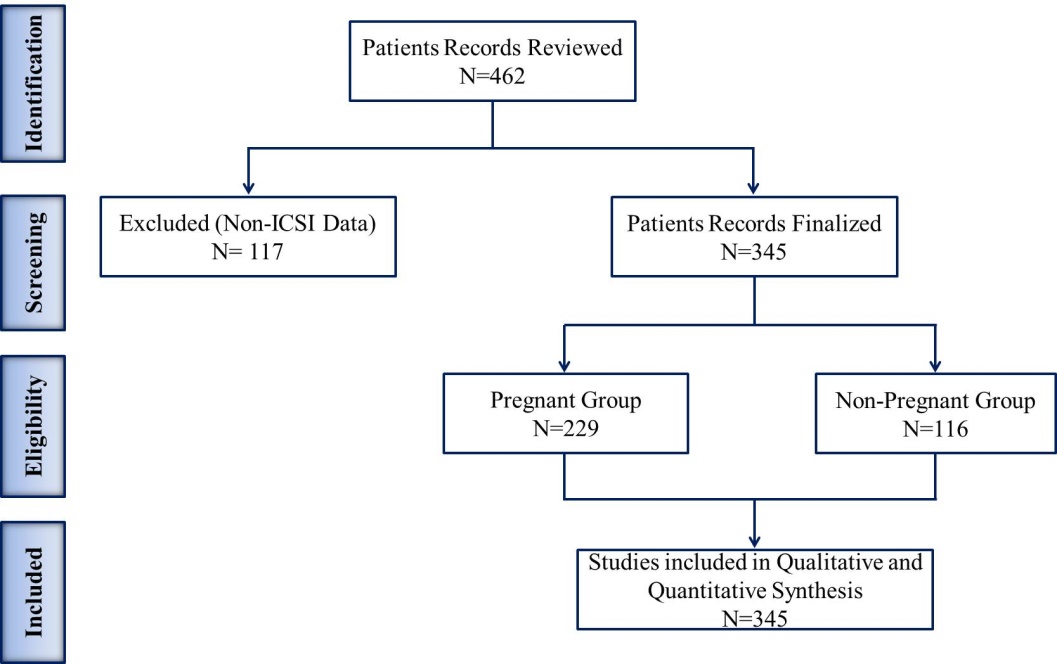
A retrospective study was conducted from January 2018 to December 2020 among 345 infertile patients who were diagnosed with endometrial polyps planned for frozen embryo transfer in ICSI cycles in our reproductive center. Hysteroscopy was performed on 345 infertile women who were suspected to have an endometrial polyp, based on a preliminary diagnosis of the endometrial polyp with transvaginal ultrasound. The age, body mass index, the type of infertility (primary or secondary), duration of infertility, menstrual pattern, were precisely evaluated in patients under study.
The endometrial polyp was divided into five types based on location: anterior, posterior, junctional, multiple, and lateral uterine wall polyps. Hysteroscopy was done under general anesthesia and the polyp was removed either by forceps under the vision and/or curettage. Immediately after the surgery, a relook hysteroscopy was performed to confirm the complete removal of the polyp. The diagnosis was confirmed by histological examination. Frozen embryo transfer is done one to three months following polypectomy. Pregnancy was confirmed by a βHCG value and the presence of a Gestation sac by transvaginal ultrasound.
Multiple linear logistic regression analysis was analysed, in which the types of Endometrial Polys were used as the dependent variable, while age, gravidity, and parity were used as independent variables. Quantitative data, such as age, BMI, duration of infertility, type of infertility, menstrual pattern, AMH, TSH, Prolactin, Estradiol, and Endometrial Thickness were expressed as the means and 95% confidence intervals (95% CIs). Differences between the pregnant and non-pregnant groups were assessed using the Mann-Whitney Utest for continuous variables and Fisher’s exact test for categorical variables. The presence of a polyp, polyp location and symptoms were compared with the Pearson Chi-Square test(χ2) and Fisher’s exact test for qualitative variables. The Chi-Square (χ2) test was used, and P<0.05 was considered to be significant. Statistical analysis was performed using SPSS 20.0 Statistical Software.
Model for adoption
In multiple linear regression, it is possible that some of the independent variables are actually correlated with one another, so it is important to check these before developing the regression model. If two independent variables are too highly correlated (r2 > ~0.6), then only one of them should be used in the regression model. Consider a multiple linear regression model with k independent predictor variables x1,..., xp and one response variable y. The formula for a multiple linear regression is:
where, for i = n observations: yi = dependent variable (Endometrial Polyp); xi = explanatory variables (Age, gravida and Parity); β0 = y-intercept (constant term); βp=slope coefficients for each explanatory variable; ϵ =the model’s error term (also known as the residuals).
We present study a simple test to determine whether there is autocorrelation (aka serial correlation), i.e. where there is a (linear) correlation between the error term for one observation and the next. This is especially relevant with time series data where the data are sequenced by time. The Durbin-Watson test uses the following statistic:
Where the ei = yi – ŷi are the residuals, n = the number elements in the sample and k = the number of independent variables.
Results
The incidence of polyps is positively related to age, gravida, and parity (p=0.000, β =2.396), with increasing incidence in low parity women (Table 1). The adjusted coefficient of determination (R2) was less than 0.003 in age and gravida and parity, which indicates that less than three per cent of the variation independent variables is ex plained by the variation in the selected independent variables. The Durbin-Watson (DW) statistics show positive autocorrelation and inconclusive position in age, gravida, and parity.
Table 1
Age, gravida, and parity related to endometrial polyps
|
Independent Variables |
Β |
Std. Error |
T |
Sig. |
|
Constant |
2.396 |
.383 |
6.254 |
.000* |
|
Age |
.009 |
.012 |
.755 |
.451 |
|
Gravida |
.038 |
.102 |
.378 |
.706 |
|
Parity |
.219 |
.655 |
.335 |
.738 |
|
R2 = 0.003 DW = 2.431 |
||||
The baseline characteristics in women who underwent polypectomy were compared. The incidence of a polyp with respect to age is 31.6±6.55years in pregnant women and 29.25±3.81 years in non-pregnant women. The p-value was statistically significant for the age group in both pregnant and non-pregnant women. According to the duration of infertility, 46% of women with polyp are with infertility less than 5 years, 31.8% of women with 6-10 years of infertility, 12.8% in women with more than 20 years of infertility. Among 76.9% of women with polyp had primary infertility and 23.1% of women had secondary infertility (Table 2).
Table 2
Baseline characteristics of patients with endometrial Polyp and ART outcomes in pregnant and non-pregnant group
In our current study AMH, prolactin, TSH, Estradiol values, endometrial thickness were compared between pregnant and non-pregnant women following the treatment for polypectomy in treatment cycle. The statistically significant difference in the p-value is found in AMH, prolactin, Estradiol value, and endometrial thickness between the two groups (Table 3).
Table 3
Hormonal variations in pregnant and non-pregnant group following polypectomy in treatment cycle
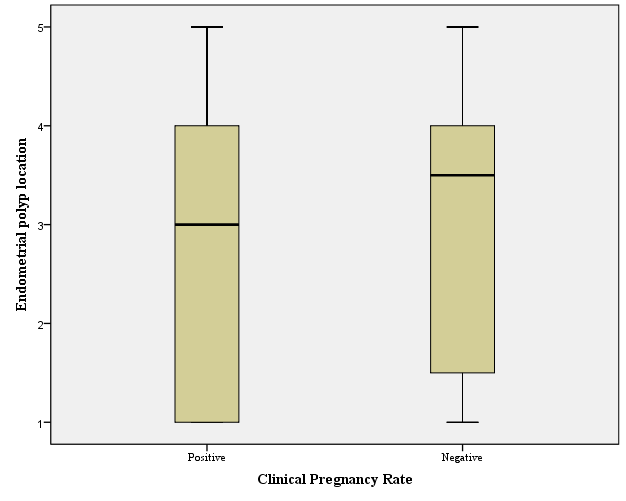
The initial diagnosis of the endometrial polyp was made by transvaginal ultrasound. Then the size, location, and a number of polyps were confirmed by diagnostic hysteroscopy and proceeded with polypectomy. Around 35.4% of polyps were multiple. 32.8% of endometrial polyps were located in the posterior uterine wall, 15.1% in the anterior wall, 9.3% were junctional and 7.5% in the lateral uterine wall. The pregnancy rate with respect to the location of polyp (0.000) is statistically significant (Figure 2, Figure 3 ).
Discussion
Among the different etiologies for infertility, endometrial polyps remain a significant cause of impaired implantation of embryo and subsequent infertility. Hence timely detection of the polyps and their removal by hysteroscopy guided polypectomy or curettage of the polyp followed by rechecking of its complete removal by subsequent hysteroscopy has shown significant improvement in the implantation rates following frozen embryo transfer in the ICSI cycles. Diagnostic hysteroscopy should be routinely used in the evaluation of infertile women10 and it remains the reliable method of removing the endometrial polyps as it reduces the risk of residual polyps.13 Our study included 345 infertile women with endometrial polyps and the pregnancy rate following polypectomy in ICSI-FET cycle was analysed. Among patients of the study group of Stamatellos et al., there were no significant differences in age, type, or duration of infertility and endometrial polyps.14 Our study showed no statistically significant difference in duration or type of infertility and endometrial polyps and the pregnancy rates.
In a retrospective cohort analysis by Reside Onalan et al. BMI is found to be an independent risk factor for endometrial polyps in patients undergoing In-vitro Fertilization.15 In their study, patients with BMI more than or equal to 30 kg/m² had a statistically significant number of endometrial polyps versus BMI less than or equal to 30 (52% vs 15%). This is in contrast to our study where BMI failed to be an independent risk factor for endometrial polyps. 337 women who became pregnant had a BMI of 24.73±4.55 in our study. In Bulent et al. study16 BMI of patients diagnosed with endometrial polyp before ICSI treatment was 26.65±5.65 kg/m² which was similar to our study result.
Yanaihara et al. study showed a higher number of multiple polyps (82%) among infertile women.17 Our study showed a higher incidence of multiple polyps (35.4%). This was similar to the study result of Guo et al. with 55.4% of infertility patients with multiple endometrial polyps.18 Though our study showed only 9.3% polyps in utero tubal junction, Shokeiret al. have reported the majority of the polyps in utero tubal junction (10%). The location of the endometrial polyp did not seem to affect the pregnancy rate in ICSI cycles in a retrospective study conducted by Bulent et al. which was similar to our study.16 In our study pregnancy rate was not determine by polyp location.
According to Shokeir et al. incidence of endometrial polyps in primary infertility is 3.8%–38.5%, and 1.8%–17% in secondary infertility.10 Valle et al. and Kalampokasetal.an reported increase in pregnancy rates after intrauterine insemination following endometrial polypectomy.19, 20 In a case-control study, Jehn Hsiahn et al. showed a higher clinical pregnancy rate of 64% following frozen embryo transfer following endometrial polypectomy.21 A randomized control study by Tu-Y-A et al. showed a clinical pregnancy rate of 64.8% in frozen embryo transfer following polypectomy.22 Varates et al. and Shokeir et al. studies also have shown a positive effect on embryo implantation after endometrial polypectomy.9, 10 Eryilmaz et al. study showed IVF outcomes were unrelated to the time interval between the hysteroscopic polypectomy. Jehm et al. recommend transfer of frozen embryos 1-2 months after polypectomy before the recurrence of endometrial polyps.23 In our study group, frozen embryo transfer was done one to three months following endometrial polypectomy, though our study was not intended to know the association between duration between polypectomy and embryo transfer and IVF outcomes. Our study showed a higher clinical pregnancy (66.37%) in 229 women out of 345 women following frozen embryo transfer after management of endometrial polyps. The possibility of a higher pregnancy rate in endometrial polyps was the main cause of infertility and implantation failure in our study sample. Hence, complete removal of polyps has improved the implantation rates and clinical pregnancy rates in our study.
Many studies have shown improved pregnancy rates following frozen embryo transfer than fresh embryo transfer. In our study, all the patients underwent vitrified embryo transfer in ICSI cycles. Afflatoin et al. and Shapiro et al study also showed similar results.23, 24 Runy Tellias et al. study resolved that newly diagnosed endometrial polypsdo not adversely affect the clinical pregnancy and live birth ratesafter fresh embryo transfer (FET) in IVF cycles.25 Check etal.study did not support the recommendation for hysteroscopic polypectomy to increase the pregnancy rates following IVF embryo transfer.26 An older study by Lass et al. concluded that small endometrial polyps do not decrease the pregnancy rate,but there is an increased rate of pregnancy loss and suggested that endometrial polypectomy prior to frozen embryo transfer might increase the take-home baby rate.27 Our study population had both smaller and bigger polyps endometrial polypectomy was done irrespective of the polyp size.
Conclusion
In the growing era of infertility bringing success in ART cycles remain a challenge for ART specialists. Wide varieties of factors pose threat to the implantation rates and clinical pregnancy rates. Hysteroscopy being a minimally invasive procedure with less complication, its use in evaluation and management of infertile women can be advocated in any suspected uterine cavity pathology. Hysteroscopic polypectomy gives promising results in infertility patients undergoing ICSI cycles prior to vitrified embryo transfer and location of polyps does not determine the pregnancy outcomes. Endometrial polyps being incidental findings in TVUS, its presence cannot be overlooked and the time management could improve the ART success rates and limit the agony of infertile couples.
Ethical Statement
Hereby, I Dr. Pradeepa Sudhakar consciously assure that the for the manuscript submitted above where in accordance with the ethical standards and informed consent was obtained from all the patients being included in the study, Prior ethical approval was obtained from the Sudha Hospital Ethical Committee.