Introduction
A dermoid cyst is a benign cystic lesion that arises from the entrapment of ectodermal and mesodermal elements. Histologically they are lined with stratified squamous epithelium with mature skin appendages found on their wall and lumen filled with keratin, hair, sweat and sebaceous glands and tooth. Common sites of occurrence are the ovaries in the reproductive age group, brain and para-nasal sinuses and scalp. Dermoid cyst in the vaginal wall is a rare finding in gynaecology.
Case Report
A 24-year-old nullipara presented to the outpatient department with an incidental finding of a right lateral vaginal cyst /? Cyst in the right ischiorectal fossa during evaluation for infertility. She had no symptoms of pain, feeling of a lump/ heaviness or dyspareunia. No history of previous vaginal surgery or trauma. On per speculum examination, a bulge was seen in the right lateral vaginal wall and the cervix was healthy. Pelvic examination revealed a large 8x6cm soft, painless swelling in the right lateral vaginal wall 2cms from the introitus with depth not made out and extending up to the right fornix. Per rectal examination showed mass occupying right paravaginal space, lateral to rectum extending into right ischiorectal fossa. Transvaginal scan showed a 74x56x60mm large well-defined hypoechoic lesion with thick internal echoes noted in the right ischio-rectal fossa. MR imaging revealed a well-defined cystic lesion measuring 74x55x45mm in the right ischio-anal and anterior perianal region. The lesion was causing significant elevation of right pelvic diaphragm and also causing compressive displacement of the urinary bladder neck (Figure 1, Figure 2). A diagnosis of right paravaginal cyst was made.
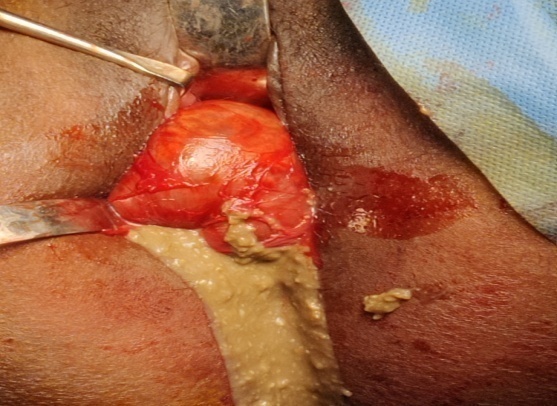
Transvaginal excision of the paravaginal cyst under general anesthesia was planned after preoperative workup. Bimanual pelvic and rectal examination was done again under anesthesia to confirm the extension of cyst. A 3cms long vertical incision was given on the right lateral vaginal mucosa overlying cyst. The cyst was separated from the vaginal mucosa by blunt and sharp dissection after infiltrating the mucosa with Dilute Adrenaline injection. Cyst was dissected from all sides. During deep dissection, the cyst wall got punctured releasing thick brownish yellow granular material looking like contents of a dermoid cyst. Cyst wall was excised completely, hemostasis secured and the dead space sutured (Figure 3, Figure 4, Figure 5). Vaginal wall was sutured with Vicryl 3-0 and pack placed in the vagina to compress the dead space. The cyst was located in the lateral vaginal wall not extending beyond the superficial perineal muscles. Vaginal pack was removed after 48hrs.
Histopathology reported as cyst wall lined with stratified squamous epithelium showing well-defined granular layer. Abundant lamellated surface keratin seen. Cyst wall showed edematous stroma with few pilosebaceous units, occasional muscle fascicles also seen with features consistent with Dermoid cyst.
Discussion
Vaginal cysts are not a rare presentation in a gynaecology OPD. Patients may be asymptomatic and incidentally diagnosed during examination, have local pain or dysperunia. Vaginal cysts are classified according to the histology and based on the lining epithelium as: mullerian cyst, bartholin cyst, epidermal inclusion cyst, endometroid cyst and unclassified variety. Mullerian cyst constitutes 30%, bartholin cyst 27.5%, epidermal inclusion cyst 25% and remaining comprise the unclassified type which includes dermoid cyst.1
Dermoid cyst has well differentiated derivatives of all three germ cell layers and is a benign tumour. The most common site for dermoid cyst are the ovaries. In 50% of the cases, it is seen in young girls and 80% of the dermoid cyst occur in the reproductive phase of life.2 Dermoid cyst is seen in rare locations like the floor of the mouth till the colon in the gastrointestinal tract.3 Paravaginal location of a dermoid cyst is rare. They constitute less than 4% of all extragonadal teratomas. It was first observed by Stokes et al4 in 1899. Curtis et al5 described an ulcerated lesion containing hair and sebaceous glands in the vaginal mucosa.
Vaginal dermoid cyst is a well demarcated lesion from the surrounding vaginal tissue and the contents are heterogenic on transvaginal sonography.6 A vaginal dermoid cyst can be confused with other cystic lesions in the vagina like the epidermal inclusion cysts which usually occur after local trauma or the mullerian cysts.
Transvaginal excision of the cyst after an MR imaging to know the extent of the cyst is the appropriate line of treatment.4, 7 Histopathology remains the gold standard in confirming the diagnosis.7, 6
Conclusion
Paravaginal dermoid cysts even though rare, should be considered as a differential diagnosis of a lateral vaginal wall cyst. Preoperative diagnosis may be difficult with transvaginal ultrasound or MRI in the absence of bone tissue or teeth. Excision under anaesthesia followed by histopathological confirmation remains the gold standard treatment. Complete resection of the cyst has excellent prognosis.