Introduction
Platelet abnormalities may precede pregnancy, develop during pregnancy coincidentally, or induced by pregnancy. Types of thrombocytopenia – Mild - 1.5 Lakhs /mm3 to 1Lakh /mm3, moderate– 1 Lakh/mm3 -50,000/mm3, severe < 50,000/mm3.3 Commonest platelet deficiency seen in obstetrics is Gestational thrombocytopenia which is 80%. Preeclampsia & HELLP syndrome - 20%, Immune thrombocytopenic purpura (ITP), others - Obstetric coagulopathies –DIC, MTP, SLE APAS, infections like – viral and sepsis syndrome, drugs, hemolytic anemias, thrombotic microangiopathies, malignancies.1 Gestational thrombocytopenia is a benign common numeric platelet deficiency disorder. Platelet counts rarely falls below 70,000/mm3. Usually there is no risk for mother or baby.3 Neonatal platelet levels should be determined at birth, further daily monitored.4 Lowest levels are recorded during days two to five post natally. When neonatal platelet count is <50,000/mm3, there is a risk of 0.5 – 1.5% of intracranial hemorrhage.5 However mode of delivery may not affect the rate of intracranial hemorrhage in thrombocytopenic newborns.6 It is most common in third trimester due to hemodilution. Normal increased splenic mass in pregnancy may also be contributory. Patients will be usually asymptomatic, there is completely negative h/o abnormal bleeding. When Platelet count falls < 80,000/mm3 we have to start evaluating. Etiology may be other than incidental or gestational thrombocytopenia.
Immune thrombocytopenic purpura has incidence 1-2/ 10,000 pregnancies. In adults – it is a chronic disease which rarely resolves spontaneously. There are two forms of presentation Primary form (ITP) idiopathic thrombocytopenic purpura, secondary form like SLE, Lymphomas, severe systemic disorders.7 Autoantibodies mediated destruction of maternal platelets by platelet associated immunoglobulin PAIgG, PAIgM, PAIgA. It is diagnosis of exclusion. Incidence in first half of pregnancy suggestive of its possibility. Here platelet counts falls below 50,000 /mm3. Patients will be usually asymptomatic, some may have easy bruising, bleeding, petechiae. Both mother and fetus will be affected, as IgG cross placenta, it may cause fetal thrombocytopenia (5- 10%) with counts <50,000/mm3. Hence, cord blood platelet counts should be monitored.
Case Reports
Case 1
A 29-year old G2P1L1 at 36 weeks of gestation admitted for severe gestational thrombocytopenia with platelet count 28,000/mm3. She gave a record showing serially falling platelet count from 36,000/mm3 to 24,000/mm3. She gave H/o petechial purpura over abdomen and legs at 32weeks of gestation and was treated with topical emollients outside for the same. She came to our hospital at 36 weeks for further management. She was started on Inj.dexamethasone 8mg IV bd as per hematologist opinion. Direct coomb’s test ANA profile viral markers, dengue serology done all were negative. Peripheral smear showed a dimorphic picture. EBV IgG was positive. Totally 5 PRBC + 4 Platelets + 16 FFP transfusion has been done during her hospital stay. Patient got labour pains. Emergency repeat lscs was done for previous lscs in labor as an indication on 28/11/2020. Inj.dexamethasone 8mg IV bd was continued. On tapering steroids dosage we noticed her platelet count was falling. Hence, hematologist was reviewed. She was diagnosed as ITP during pregnancy. Her last platelet count was 79,000/mm3 on discharge. Even after 1 year of delivery she requires steroids for her platelets to be maintained. Currently she is on T. Prednisolone 20 mg per day. Monthly platelet count monitoring is done. Her present platelet count is 4.7 L/ mm3.
Case 2
A 25-year-old primigravida at 40wks + 1day of gestation was admitted for platelet count 46,000/mm3. She was diagnosed to be severe gestational thrombocytopenia and was induced for postdatism. She was delivered by Emergency LSCS for failed induction. Inj.Methylprednisolone 40mg IV od was started. Intraop two platelet transfusions were done. She became normal after post-operative day three with normal platelet counts 2.9 L/mm3 and was discharged. She is doing well now.
Case 3
A 33-year old G2A1 at 39 weeks of gestation was diagnosed as moderate gestational thrombocytopenia with platelet count -93,000/mm3 on routine screening. Induction of labor was done for decreased fetal movements and emergency Lscs was done for failed induction. Intraop two platelet transfusions were done as there was excess intraop blood loss. On post op day four her platelets became normal 1.5 Lakhs/mm3 without any requirement of steroids.
Discussion
During study period we have observed that cases of gestational thrombocytopenia attaining the normal platelet counts on the post natal day three or four, and limitations of the manifestations were studied. Usually there is no risk for mother or baby. In these cases a platelet count should be obtained before epidural anesthesia, in most of the guidelines reference value is around 75,000-80,000/mm3 for providing anaesthesia.8 There is a theoretical concern over the risk of epidural hematoma with lower platelet values. Pregnancy does not worsen the outcome of ITP, but there may be adverse fetal and maternal consequences in some cases. Spontaneous bleeding with platelets <20,000/mm3 and the risk of internal bleeding if platelets <10,000/mm3 were reported. When platelets count is < 30,000/mm3 steroids or IVIG is recommended.9 In our first case with platelets 28,000/mm3 we have ruled out all the causes of thrombocytopenia and started the patient on steroids IV Dexamethasone and found a fall in platelets on tapering steroids hence steroids were continued throughout the pregnancy and even after seven months of delivery she continues with steroid intake and monthly platelet monitoring were done. Whereas the other two cases did not require any further follow up or management. Many studies were conducted on evaluating the causes of thrombocytopenia in pregnancy and the reference range for epidural anaesthesia also brought up in many studies, which is taken for management during pregnancy.
Conclusion
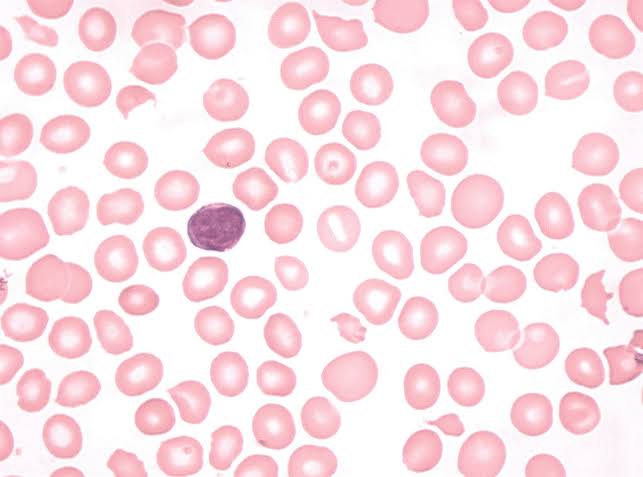
In conclusion, Gestational thrombocytopenia is the most common cause of thrombocytopenia during pregnancy, but other underlying causes must be considered as well. A thorough history and physical examination rules out most causes. In blood – remainder of CBC and peripheral smear will help us to rule out other causes such as pancytopenia and platelet clumping associated with psuedothrombocytopenia. If there is no antecedent history and platelet count > 70,000/mm3 to 1.5 lakhs/mm3–it is more likely Gestational thrombocytopenia. If there is pre existing history with platelets <50,000/mm3 - it is likely ITP. There is a positive correlation between thrombocytopenia with adverse fetomaternal outcome. Hence serial platelet monitoting should be done. Proper antenatal care and institutional deliveries enable obstetricians to diagnose the condition at early stage and intervene which results in a better outcome. Optimum management of ITP in pregnancy requires collaboration between the obstetrician, hematologist and paediatrician.10