- Visibility 251 Views
- Downloads 62 Downloads
- Permissions
- DOI 10.18231/j.ijogr.2023.029
-
CrossMark
- Citation
Role of prophylactic use of tranexamic acid in reducing blood loss during caesarean section in a tertiary care hospital
Abstract
Background: Postpartum Haemorrhage (PPH) is an important cause of maternal death and severe maternal morbidity. Compared to vaginal delivery, women undergoing caesarean delivery incur the highest risk of PPH and haemorrhage related morbidity. Furthermore, evidence suggests that PPH during caesarean delivery is occurring more frequently.
Objective: To study the effect of low dose intravenous tranexamic acid in reducing blood loss during Caesarean section.
Materials and Methods: This randomized control trial among 50 antenatal women aged >18 years undergoing Lower segment caesarean section in tertiary care centre. They were divided into Study group and control group. Study group received 1gm iv tranexamic acid and the Control group did not receive tranexamic acid. Data was entered in Microsoft Excel data sheet (MS-Excel) and analysed using commercially available SPSS 23 software package. MS Excel and MS word was used to obtain various types of graphs such as bar diagram.
Results: Among the study population who underwent Lower section caesarean section in our study, we found that the requirement of additional oxytocin was nil with tranexamic acid group (p value<0.02). There were no side effects observed with the group administered tranexamic acid (p value<0.01). The difference in mean of bleeding from placental delivery to end of Caesarean Section, End of Caesarean Section to 2 hrs Postpartum was statistically significant (p value <0.05). The fall in Hb% between the two groups was significant, thereby showing the benefits of Tranexamic acid.
Conclusion: Tranexamic acid significantly reduces the amount of blood loss during and after lower segment caesarean section. It was not associated with any significant side effects and complications. It can be used effectively in all women undergoing caesarean section to reduce the postpartum Haemorrhage thereby reducing the maternal morbidity and mortality.
Introduction
Caesarean section (CS) rates have increased to 25 to 30% all over the world. Obstetric haemorrhage accounts for 20-25% of maternal mortality and morbidity. The most common complication of caesarean section is primary and secondary haemorrhage (20%). It leads to increase in maternal mortality and morbidity.[1]
The most significant challenge that an obstetrician faces during delivery is managing the placental separation that takes place during the third stage of labor. Myometrial contractions cause a significant constriction of blood vessels in the placental bed; however, adequate fibrin formation is also required for the process to be successful.
Because pregnancy is always represented as a hypercoagulable state, many physiological adaptations take place during pregnancy, and the hemostatic challenge is met in almost all pregnant women. During pregnancy, there is an increase in the concentration of many factors that contribute to blood clotting, including factors II, VII, VIII, IX, and XII. During pregnancy, a woman's body naturally produces fewer factors XI and XIII, which results in a lower concentration of clotting factors overall. This phenomenon is most prevalent in the third trimester of pregnancy.[2]
Tranexamic acid (TXA) is a synthetic lysine aminoacid derivative. It acts as an antifibrinolytic agent by blocking the lysine binding site on plasminogen molecules in a manner that is reversible. This reduces the rate at which hemostatic fibrin is dissolved by plasmin, which is the process that causes blood clots to break down.[3] This results in the lysine receptors binding sites of plasmin for fibrin being well occupied by tranexamic acid, which prevents the binding of fibrin molecules and, as a result, preserves and stabilizes the fibrin matrix.[4]
Absorption following a single dose of oral administration, the peak concentration in plasma is reached in about three hours on average. On distribution, the plasma concentration of tranexamic acid is 30mg/L following an intravenous injection of 10mg/kg of tranexamic acid in pregnant women. Only a small portion of the drug is converted into its active form. The majority of it is flushed out of the body within the first ten hours, followed by other fractions.[5] The half-life is approximately two hours. It has minimum side effects. Tranexamic acid is also used in various conditions like menorrhagia, Bleeding associated pregnancy, all gynecological procedures, traumatic hemorrhage and other surgical procedures.[6]
Hemorrhage that occurs during pregnancy is responsible for nearly 30 percent of all cases of maternal mortality. Clinicians continue to rely on visual estimates to determine the amount of postpartum blood loss, despite the fact, these estimates are frequently found to be inaccurate. Estimating the amount of blood lost during the postpartum period can be done using any one of a number of different methods. E.g.- Visual Assessment, Direct and standard measuring jar, Rubberized Blood Mat, Kelly’s Pad, Gravimetric method and Laboratory based methods.[7], [8]
When we fail to recognize the excessive blood loss that occurs during child birth, if early intervention is not initiated, obstetric hemorrhage can lead to death, which is the worst complication of pregnancy. The objective of this study was to study the effect of intravenous Tranexamic acid in reducing blood loss in patients undergoing Lower Segment Caesarean Section.[9]
Materials and Methods
This study was a Randomised Controlled Trial done in all the antenatal mothers aged >18yrs who underwent Caesarean section in the Department of Obstetrics and Gynaecology, in a tertiary care centre, Chengalpattu District, Tamil Nadu. This study was done in 50 antenatal patients who were satisfying the eligibility criteria after Institutional ethical committee approval number- 2021/662 was obtained.
Antenatal mothers >18yrs, Full term primigravida or Multigravida with singleton pregnancy undergoing Lower segment Caesarean section at Obstetrics and Gynaecology department were included and patient with Medical and surgical co-morbidities, History of thromboembolic disorders, complicated pregnancy, bleeding diathesis, those who are allergic to tranexamic acid, multiple pregnancy and polyhydramnios were excluded.
The patients were randomly categorized into Group A and Group B in the order of admission. All odd numbers were assigned in Group A and even numbers were assigned in Group B. Group A was considered as a study group and received 1gm intravenous tranexamic acid before incision and Group B was considered as a Control group who did not receive tranexamic acid before incision. Informed written consent was obtained from all the participants before proceeding.
Tranexamic acid was administered 15 to 20 minutes before incision in a dosage of one gram intravenously and slowly infused over 5-10 minutes, in addition to Oxytocin after the delivery of baby. Blood was collected into the suction container after the placental separation, thus excluding the collection of amniotic fluid into the suction container, so that the collected blood is only from that which has occurred after placental delivery.
All the soaked Gauge pads and operation table sheets were weighed before and after surgery. The measurement was done in two different periods. One from the time of placental separation to the end of surgery. The other from the end of surgery to two hours postpartum.
Quantity of blood loss = (weight of used material + weight of unused material) - (weight of all material prior to surgery) + volume collected in the suction container after placental delivery.
Evaluation of effectiveness of Tranexamic acid was given by:
Efficacy of the drug -Amount of blood loss and fall in hemoglobin.
Safety of the drug – Monitoring of vitals, general side effects and laboratory findings.
Statistics and analysis of data
Data was entered in Microsoft Excel data sheet (MS-Excel) and analysed using commercially available SPSS 23 software package. Chi-square test was used as test of significance for qualitative data. Continuous data was represented as mean and SD. Graphical representation of data: MS Excel and MS word was used to obtain various types of graphs such as bar diagram. P value (Probability that the result is true) of <0.05 was considered as statistically significant after assuming all the rules of statistical tests. Statistical software: MS Excel, SPSS version 22 (IBM SPSS Statistics, Somers NY, USA) was used to analyse data.
Results
Among the study population, the mean difference of BMI was 26.4±2.75 in Group A and 27.52±3.07 in Group B, P value was 0. 181. The mean difference of Age among the study population was 25.68±3.86 in Group A and 24.96±3.83 in Group B, P value was 0.511. The mean difference of period of gestation between both the groups was 38.86±0.65 and 38.86±0.79 and P value was 0.999. Comparison of Socioeconomic status, place of living and occupation between the two groups was done. It was not statistically significant. P value >0.05 in our study.
|
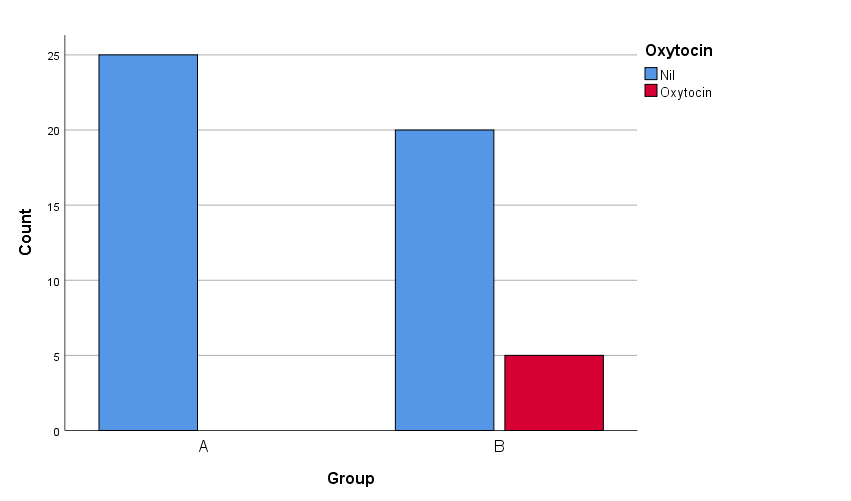
Use of Additional Oxytocin |
Group |
Chi square |
P value |
|
|
A (N=25) |
B (N=25) |
|||
|
Nil |
25 (100%) |
20 (88%) |
5.556 |
0.02 |
|
Oxytocin |
0 (0%) |
5 (12%) |
|
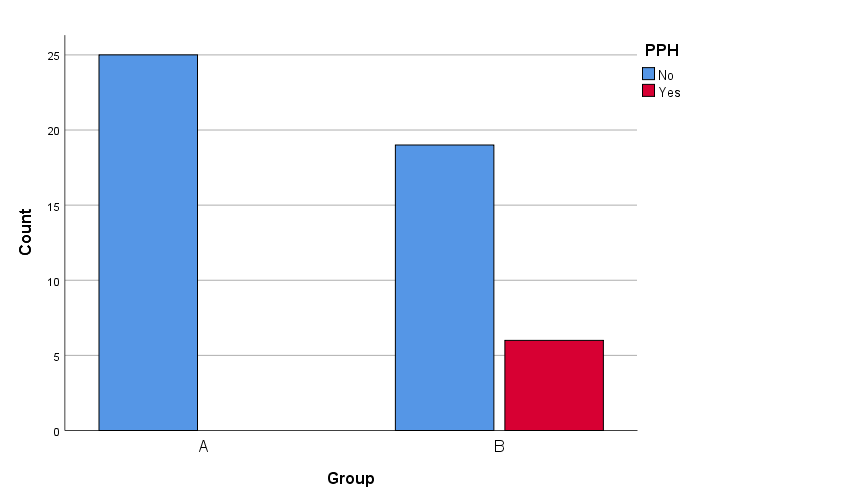
Complication |
Group |
Chi square |
P value |
|
|
A (N=25) |
B (N=25) |
|||
|
Nil |
25 (100%) |
19 (88%) |
6.818 |
0.01 |
|
PPH |
0 (0%) |
6 (12%) |
Among the study population, the difference in proportion of complication between study group was statistically significant. (p value <0.05).
|
Parameter |
Group (Mean± SD) |
P value |
|
|
A (N=25) |
B (N=25) |
||
|
Placental delivery to end of CS |
429.6 ± 16.2 |
679.2 ± 301.2 |
<0.001 |
|
End of CS to 2 hrs Postpartum |
40.4 ± 6.11 |
68.8 ± 14.53 |
<0.001 |
|
Total |
470 ± 14.14 |
748 ± 315.73 |
<0.001 |
|
Fall in Hb% (gm/dl) |
0.48 ± 0.23 |
1.22 ± 0.71 |
<0.001 |
The difference in mean of bleeding from placental delivery to end of CS, end of CS to 2 hrs postpartum, total of both, Fall in Hb% (gm/dl) between study group was statistically significant. (p value <0.05).
Discussion
This was a randomized controlled trial conducted among the antenatal women aged > 18 years who had underwent lower segment caesarean section at the Department of Obstetrics and Gynaecology, Tertiary Care Centre, Nellikuppam, Ammapettai for about 18 months. One group received tranexamic acid while the other group did not. This was carried out to study the effect of intravenous low dose Tranexamic acid in blood loss reduction during caesarean section. Sample size was based on the article 11.[10]
Among the study population, the mean difference of BMI, Age, period of gestation between study group was not statistically significant. (p value >0.05). The mean age of the participants was 25 years. This was similarly supported by Gautam et al. where they found majority of the participants was around the age group of 26 years.[11] We found that the mean gestational week of the women was 39 weeks. This was corroborated by Pirjani et al. where they observed the similar results.[12]
Parity and caesarean section
Among the study population with parity, in group A 10 (40%) of them were primi, 9 (36%) of them were G2P1L1 and in group B 9 (36%) of them were primi, 12 (48%) of them were G2P1L1. This was supported by the study conducted by Rydahl et al. As a mother's age increased, caesarean sections rates increased. Only a minimum change in risk was seen when maternal and obstetric risk factors were taken into account.[13]
Use of oxytocin is lesser required with tranexamic acid
In our study there was a significant difference in the need of additional oxytocin between the two groups and the difference was statistically significant. (p value <0.05). In our study, we found that the requirement of oxytocin was nil with tranexamic acid group. This was supported by Mova et al. In the TXA group the mean intraoperative blood loss and the mean postoperative blood loss was considerably lower when compared with than those in the control group (262.5± 39.6 vs. 404.7 ±94.4 mL and 67.1± 6.5 vs. 141.0 ±33.9 mL, respectively; P 0.001). In the tranexamic acid group, oxytocin administration was considerably lower than in the control group (39 ±5.8 vs. 43 ±5.4 units; P=0.001). They concluded that tranexamic acid given intravenously reduced intraoperative and postoperative blood loss as well as oxytocin administration in patients having caesarean deliveries.[14]
Complications
In our study, we found that there were no complications like PPH with the group administered tranexamic acid. We found a statistically significant (p value <0.05) difference in the complication rate between two groups. Sharma et al. found that both groups were comparable to one another, and there was a little statistical difference between them. Tranexamic acid lessened complications during and after caesarean section.[15]
Side-effects
We found that there were no side effects with tranexamic acid. Among the study population, the difference in proportion of side effect between study group was not statistically significant. (p value >0.05). Sharma et al. also highlighted that the blood loss during and following a lower segment caesarean section is greatly lessened with tranexamic acid. Tranexamic acid use was not linked to any complications or adverse effects like thrombosis, nausea, vomiting, or diarrhoea.[15]
Comparison of mean of bleeding from placental delivery to end of CS between group
In our study, we found that the difference in mean of bleeding from Placental delivery to CS end, CS end to 2 hrs Postpartum, the Total, fall in Hb% (gm/dl) before delivery and 24 hours after delivery between the study groups was statistically significant. (p value <0.05). This was supported by the study conducted by Shahid et al. Blood loss from placental delivery until the end of LSCS was reduced significantly by tranexamic acid, falling to 429.6 16.2 ml in the TXA group as opposed to 679.2 301.2.72 ml in the placebo group (p 0.001). Additionally, blood loss from the conclusion of LSCS to two hours after delivery was reduced and was 40.4 6.11 ml in the TXA group and whereas it was only found to be 68.8 14.53 ml in the placebo group (p = 0.188), this difference was statistically significant. They found that the blood loss following the caesarean section was dramatically reduced intraoperative during the LSCS. TXA can be administered efficiently and safely to reduce intraoperative blood loss in LSCS patients.[16]
Blood loss and transfusion requirements
Similar to the findings in our study, Gupta et al found that the Tranexamic acid has been efficiently used as a preventative measure to limit blood loss and transfusion requirements during surgery without causing any negative side effects or thrombosis complications.[17]
Conclusion
Tranexamic acid significantly reduces the amount of blood loss during and after lower segment caesarean section. It was not associated with any significant side effects and complications. It can be used effectively in all women undergoing caesarean section to reduce the postpartum Haemorrhage thereby reducing the maternal morbidity and mortality.
Source of Funding
None.
Conflict of Interest
None.
References
- Kietpeerakool C, Lumbiganon P, Laopaiboon M, Rattanakanokchai S, Vogel JP, Gülmezoglu A. Pregnancy outcomes of women with previous caesarean sections: Secondary analysis of World Health Organization Multicountry Survey on Maternal and Newborn Health. Sci Rep. 2019;5(1):1-9. [Google Scholar]
- Soma-Pillay P, Catherine N, Tolppanen H, Mebazaa A. Physiological changes in pregnancy. Cardiovasc J Afr. 2016;27(2):89-94. [Google Scholar]
- Mccormack P. Tranexamic acid. Drugs. 2012;72(5):585-617. [Google Scholar]
- Levy J, Koster A, Quinones Q, Milling T, Key N. Antifibrinolytic therapy and perioperative considerations. Anesthesiology. 2018;128(3):657-70. [Google Scholar]
- Muhunthan K, Balakumar S, Navaratnaraja T, Premakrishna S, Arulkumaran S. Plasma Concentrations of Tranexamic Acid in Postpartum Women After Oral Administration. Obstet Gynecol. 2020;135(4):945-8. [Google Scholar]
- Ghimire S, Ravi S, Budhathoki R, Arjyal L, Hamal S, Bista A. Current understanding and future implications of sepsis-induced thrombocytopenia. Eur J Haematol. 2021;106(3):301-5. [Google Scholar]
- Toledo P, Mccarthy R, Hewlett B, Fitzgerald C, Wong C. The accuracy of blood loss estimation after simulated vaginal delivery. Anesth Analg. 2007;105(6):1736-40. [Google Scholar]
- Larsson C, Saltvedt S, Wiklund I, Pahlen S, Andolf E. Estimation of blood loss after cesarean section and vaginal delivery has low validity with a tendency to exaggeration. Acta Obstet Gynecol Scand. 2006;85(12):1448-52. [Google Scholar]
- Mielke R, Obermeyer S. The use of tranexamic acid to prevent postpartum hemorrhage. J Midwifery Womens Health. 2020;65(3):410-6. [Google Scholar]
- Lakshmi S, Abraham R. Role of prophylactic tranexamic acid in reducing blood loss during elective caesarean section: a randomized controlled study. J Clin Diagn Res. 2016;10(12):17-21. [Google Scholar]
- Gautam P, Karki C, AA. Robson’s Group 2 Criteria among Total Caesarean Sections in a Tertiary Care Hospital: A Descriptive Cross-sectional Study. JNMA J Nepal Med Assoc. 2021;59(243):1094-1101. [Google Scholar]
- Pirjani R, Afrakhteh M, Sepidarkish M, Nariman S. Elective caesarean section at 38-39 weeks gestation compared to > 39 weeks on neonatal outcomes: a prospective cohort study. BMC Pregnancy Childbirth. 2018;18(1). [Google Scholar]
- Rydahl E, Declercq E, Juhl M, Maimburg R. Cesarean section on a rise-Does advanced maternal age explain the increase? A population register-based study. PLoS One. 2019;14(1). [Google Scholar]
- Movafegh A, Eslamian L, Dorabadi A. Effect of intravenous tranexamic acid administration on blood loss during and after cesarean delivery. Int J Gynaecol Obstet. 2011;115(3):224-6. [Google Scholar]
- Sharma R, Najam R, Misra M. Efficacy of tranexamic acid in decreasing blood loss during and after cesarean section. Biomed Pharmacol J. 2015;4(1):231-5. [Google Scholar]
- Shahid A, Khan A. Tranexamic acid in decreasing blood loss during and after caesarean section. J Coll Physicians Surg Pak. 2013;23(7):459-62. [Google Scholar]
- Gupta K, Rastogi B, Krishan A, Gupta A, Singh V, Agarwal S. The prophylactic role of tranexamic acid to reduce blood loss during radical surgery: A prospective study. Anesth Essays Res. 2012;6(1):70-3. [Google Scholar]
- Abstract
- Introduction
- Materials and Methods
- Results
- Discussion
- Parity and caesarean section
- Use of oxytocin is lesser required with tranexamic acid
- Complications
- Side-effects
- Comparison of mean of bleeding from placental delivery to end of CS between group
- Blood loss and transfusion requirements
- Conclusion
- Source of Funding
- Conflict of Interest
- References
How to Cite This Article
Vancouver
Mathumitha K, Gopalan U. Role of prophylactic use of tranexamic acid in reducing blood loss during caesarean section in a tertiary care hospital [Internet]. Indian J Obstet Gynecol Res. 2023 [cited 2025 Oct 28];10(2):126-130. Available from: https://doi.org/10.18231/j.ijogr.2023.029
APA
Mathumitha, K., Gopalan, U. (2023). Role of prophylactic use of tranexamic acid in reducing blood loss during caesarean section in a tertiary care hospital. Indian J Obstet Gynecol Res, 10(2), 126-130. https://doi.org/10.18231/j.ijogr.2023.029
MLA
Mathumitha, K, Gopalan, Ushadevi. "Role of prophylactic use of tranexamic acid in reducing blood loss during caesarean section in a tertiary care hospital." Indian J Obstet Gynecol Res, vol. 10, no. 2, 2023, pp. 126-130. https://doi.org/10.18231/j.ijogr.2023.029
Chicago
Mathumitha, K., Gopalan, U.. "Role of prophylactic use of tranexamic acid in reducing blood loss during caesarean section in a tertiary care hospital." Indian J Obstet Gynecol Res 10, no. 2 (2023): 126-130. https://doi.org/10.18231/j.ijogr.2023.029
