Introduction
Non-tubal ectopic pregnancies being rare but potentially life-threatening conditions encountered by gynecologists. Incidence ranges between 5-8.3% of all ectopic pregnancies.1 The incidence has increased in last few decades due to increased incidence of caesarean section, assisted reproductive techniques, hysterotomy, dilatation & curettage and certain tubal and uterine surgeries like myomectomy, metroplasty, manual removal of placenta, genital tract infection, previous history of ectopic pregnancy, intrauterine devices, endometriosis, Asherman’s syndrome and smoking. The frequency of cervical ectopic pregnancy is <1% of all ectopic pregnancy,2 while caesarean scar pregnancy and interstitial pregnancy is around 4.2% and 2-11% respectively.3, 4 The commonest symptom is vaginal bleeding which could be mild to profuse and painless. Beta-hCG levels and TVS ultrasound are done to confirm diagnosis. Site of implantation in ectopic pregnancy determines the severity.2 Early diagnosis and definitive treatment are essential to reduce the immediate and delayed complications, maternal morbidity and mortality.1 In this article, we report management multiple cases of non-tubal ectopic pregnancy at our hospital, briefing and outlining the best possible fertility sparing treatment in vitally and hemodynamically stable patients.
Case 1: Cesarean Scar Ectopic Pregnancyunderwent Exploratory Laparotomy
A 29-year-old female, gravida 4, Para 3, Living 3 with 9.4 weeks of gestation with history of previous 3 full term caesarean section presented with spotting per vagina and pain in abdomen for 2 days and a positive urine pregnancy test. Ultrasound revealed a single live pregnancy of 9.4 weeks at anterior portion of uterine isthmus with thinning of myometrium at the previous uterine scar with empty cervical canal. Beta- hCG value was 28210mIU/L. Patient underwent exploratory laparotomy. Uterus was bulky around 12 weeks size with no abnormality in adnexa. Uterus adherent to anterior abdominal wall, adhesiolysis done. Urinary bladder was identified, mobilized and pushed down. Hysterotomy incision taken and G-sac with placenta excised in toto and sent for histopathology. Beta-hCG levels reduced to 3028mIU/L and became undetectable on subsequent follow-up. Histopathology confirmed the presence of decidual and chorionic tissue.
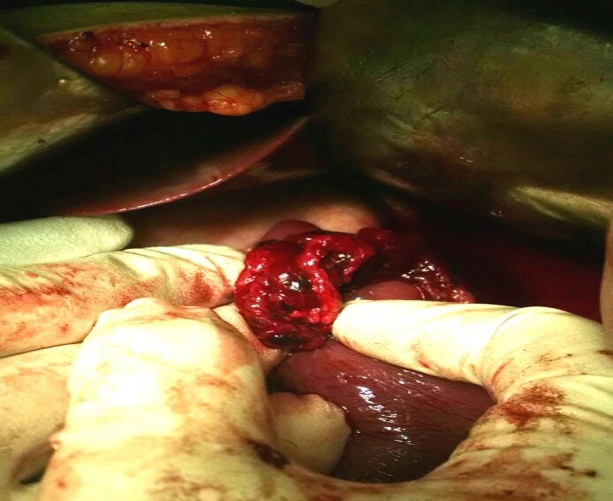
Case 2: Splenic Ectopic Pregnancy
19-year-old female, Primigravida, 7 weeks of gestation presented with abdominal pain and tenderness, minimal vaginal brownish discharge and positive urine pregnancy test. Ultrasound suggestive of intraperitoneal hemorrhage, no tubo-ovarian mass seen with empty uterus and thick endometrium. Patient was hemodynamically stable. On admission, Beta-hCG was 10,000 mIU/ml. Exploratory laparotomy was done. Hemoperitoneum of approximately 1200cc noted. Uterus, bilateral fallopian tubes and ovaries were normal and no evidence of tubal or ovarian ectopic pregnancy was found. Splenic pregnancy was diagnosed intraoperatively as soft, irregular, chorionic villous/trophoblastic like tissue, approx. 3X9X2 cm was attached on supra-lateral surface of spleen; tissue was removed and hemostasis was obtained. Serum Beta-hCG was repeated on post-op day 4 which was 802.4 mIU/ml and after a week, serum Beta-hCG levels were undetectable. Histopathology revealed chorionic villi invading splenic parenchyma.
Case 3: Interstitial Ectopic Pregnancy
A 26-year-old, Gravida 2 para 1 Living 1 with previous one full term LSCS presented with complaints of pain in abdomen and amenorrhea for 1 month. Transvaginal ultrasound done suggestive of right chronic interstitial ectopic pregnancy. Beta-hCG value was 16,814 mIU/mL. Patient was taken up for emergency exploratory laparotomy. Ectopic gestation measuring 4X4 cm visualized on right cornua of uterus with no evidence hemoperitoneum. Right sided fallopian tube and ovary was normal. Ectopic pregnancy was excised, and uterine wall was sutured in double layer. Samples sent for histopathology confirmed the diagnosis. Beta-hCG repeated on day 7 was 5,006 mIU/mL and on day 14 value was 856 mIU/mL and became negative in subsequent follow-up.
Case 4: Cervical Pregnancy Managed with Methotrexate
A 30-year-old female, Primigravida, 6 weeks of gestation presented with history of bleeding per vagina since last 15 days and positive urine pregnancy test. On vaginal examination, cervix was ballooned up and smeared with blood, uterus was approximately 8 weeks size. Beta-hCG value was 27112mIU/ml on admission. Trans-vaginal ultrasound showed gestational sac of 0.6 cm diameter was attached to anterior wall cervix, fetal pole was seen with no cardiac activity. 6 doses of Inj. Methotrexate 1mg/kg intramuscular was given as per body weight alternating with Inj. Leucovorin 0.1mg/kg IM (6 doses). Beta-hCG values after initiation of chemotherapy were 858.5 mIU/ml on 15th day. 550mIU/ml on 22nd day, 200mIU/ml on 30th day and negative after 55 days with normal pelvis sonography.
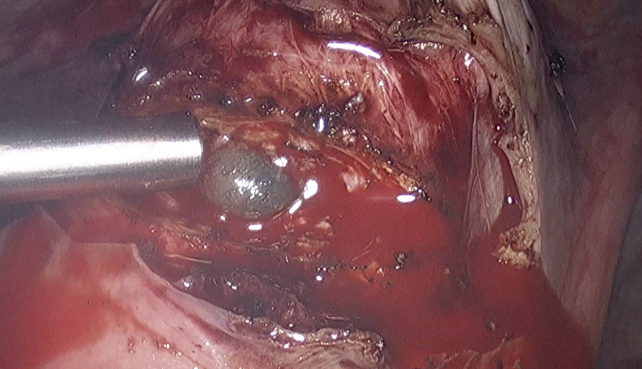
Case 5: Cesarean Scar Ectopic Pregnancy Managed Through Laparoscopy
A 30-year-old female, gravida 2, living 1, para 1, presented with bleeding per vagina with pain in abdomen for 2 days with history of term lower segment caesarean section 7 years back and a positive urine pregnancy test. Abdominal ultrasound revealed a single live pregnancy of 7 weeks 4 days at lower uterine segment with thinning and stretching of myometrium at scar site. Doppler showed significant blood flow in the area of the mass. Beta-hCG value was 85,000mIU/mL. Patient underwent diagnostic and operative laparoscopy. Uterus was seen soft, bulky around 10 weeks size. Bilateral adnexa were normal. Bladder was adherent to anterior uterine wall. Gestational sac densely adhered to scar. Dark reddish tissue suggestive of products of conception were removed. Blood loss was limited. Beta-hCG levels dropped and finally became undetectable on subsequent follow-up. Histopathology revealed decidual and chorionic villi which was consistent with ectopic pregnancy.
Case 6: Cesarean Scar Ectopic Pregnancy Managed with Methotrexate
A 34-year-old, Gravida 3, Para 2, Living 2 with history of previous 2 full term LSCS at 5 weeks of gestation presented with positive urine pregnancy test. On vaginal examination, uterus was approximately 6 weeks size. Beta-hCG value was 910.8mIU/ml on admission. Trans-vaginal ultrasound showed an irregular gestational sac of 12.5X12.3X8.9 mm within anterior myometrium at the site of caesarean scar with a high color doppler flow around mass. 3 doses of Inj. Methotrexate 1mg/kg intramuscular was given as per body weight alternating with Inj. Leucovorin 0.1mg/kg IM. Beta-hCG values after initiation of chemotherapy were 220 mIU/ml on 15th day. 112.6 mIU/ml on 22nd day, 45.19 mIU/ml on 30th day and negative after 55 days with normal pelvis sonography.
Case 7: Ruptured Cesarean Scar Ectopic Pregnancy Underwent Exploratory Laparotomy
A 28-year-old Gravida 3 Para 2 Living 2 with history of previous 2 full term LSCS with 6 weeks of amenorrhea with ultrasound suggestive of cesarean scar ectopic gestation. Patient was hemodynamically stable at the time of admission. Beta-hCG on admission was 25,780 mIU/Land value repeated on next day was 32,440 mIU/L. Patient developed tachycardia and tenderness in abdomen during the hospital stay, for which she was taken up for exploratory laparotomy. Uterus was bulky with clots around the uterus. Hemoperitoneum of 300ml present. There was presence of gestational sac in the anterior isthmic portion. Clots were removed, the defect on anterior uterine wall was repaired. Beta-hCG repeated on 4th post-operative day was 10,670 mIU/L and levels on Day 7 were 1,060 mIU/L which finally became undetectable on subsequent follow-up. Histopathology report confirmed the presence of chorionic tissue.
Case 8: Cervical Pregnancy Managed with Surgical Intervention
A 29-year-old Gravida 2 para 1 living 1 with previous full term vaginal delivery presented with complaints of spotting per vagina (on & off) for 1 week history of 6 weeks of amenorrhea. No associated history of abdominal pain and urinary symptoms. Urine pregnancy test was positive and baseline beta-hCG done which was 7520 mIU/L. Speculum examination showed no heavy bleeding, however, continuous trickle of blood was present. Vaginal examination done in which cervix was bulky, soft and ballooned up, however, uterine size was normal with no adnexal pathology. TVS ultrasound done was suggestive an empty uterine cavity and a bulky cervix with g-sac in cervical canal with color doppler showing extensive blood supply. However, no cardiac activity was noted. Patient was admitted. 3 doses of Inj. Methotrexate were given at dose of 1mg/kg body weight. Serial beta-hCG and ultrasound monitoring was done. Day 4 and Day 7 beta-hCG levels were 5450 mIU/L and 4270 mIU/L respectively. Ultrasound after 1 week was suggestive of echogenic mass measuring 3.5 x 3.2 x 3cm. Patient underwent uneventful evacuation and curettage. Patient was discharged with subsequent follow-up of beta-hCG levels. 6 weeks later, beta-hCG was less than 5mIU/L with a normal TVS ultrasound. Histopathology report was consistent with diagnosis cervical pregnancy showing chorionic villi and decidual tissue with adjacent endocervical glands and tissues.
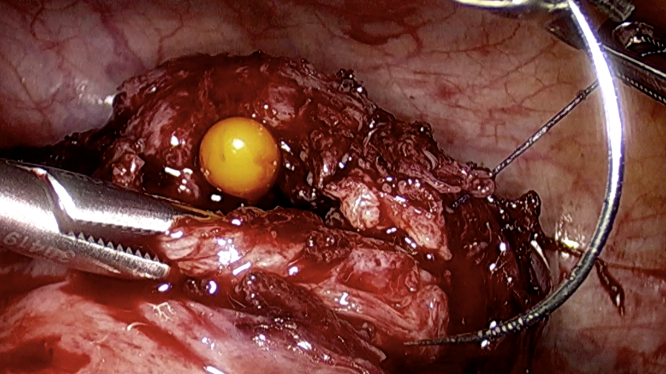
Case 9: Ovarian Ectopic Pregnancy Managed with Exploratory Laparotomy
A 36-year-old Gravida 4 para 2 living 2 abortion 1 with previous full term vaginal delivery presented with complaints of pain in abdomen over right iliac region along with spotting per vagina with 10 weeks of amenorrhea. Urine pregnancy test was positive and baseline beta hCG was done which was 62,830 mlU/L. Speculum examination showed spotting per vaginum. Vaginal examination done in which uterine size was normal with right sided forniceal fullness indicating an adnexal pathology. Ultrasound was done which was suggestive of an empty uterine cavity and a right sided cystic ovarian mass measuring 8 x 7.3 cms. Cardiac activity was noted. Patient was taken up for exploratory laparotomy. Right ovary appeared hyperemic with increased vascularity. Right sided salphingo-oophorectomy with excision of mass was done. Gestational sac with fetus & placenta visualized. Findings confirmed on histopathology. Post operative recovery of the patient was normal. Beta hCG was repeated on post operative day 7 and 14 with values being 150 mIU/L and 10 mIU/L respectively.
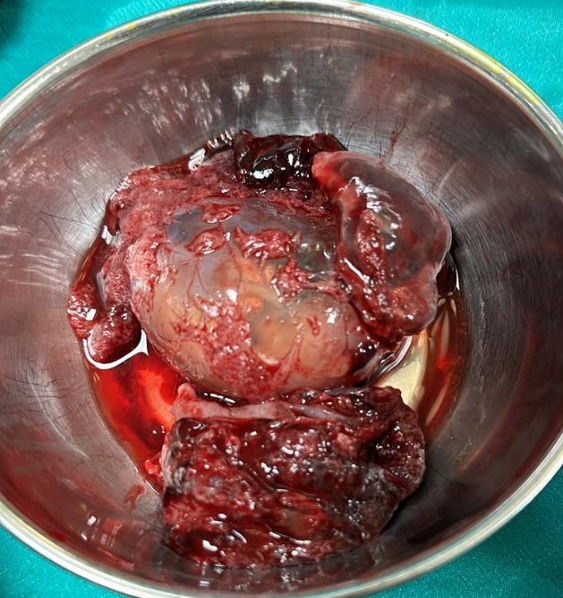
Case 10: Cervical Pregnancy Managed with Obstetric Hysterectomy
A 26-year-old Gravida 2 para 1 living 2 with previous full term vaginal delivery with 9 weeks of amenorrhea presented with complaints of uncontrolled cervical bleeding with a history of MTP pills consumption and a dilatation and curettage done in view of threatened abortion. Patient was vitally unstable, with pulse rate of 130 beats per minute, blood pressure of 90/70 mm of Hg. Clinical findings concurrent with Hemorrhagic shock secondary to rupture of cervical ectopic pregnancy. Hence, patient was resuscitated and taken up for exploratory laparotomy under general anesthesia. Obstetric hysterectomy was done with bilateral salpingectomy. Post operative recovery was normal. Specimen was sent for histopathological examination. Histopathology report was consistent with diagnosis cervical pregnancy showing chorionic villi and decidual tissue with adjacent endocervical glands and tissues.
Discussion
Management of non-tubal ectopic pregnancy can be a massive challenge for gynecologist because of its rare occurrence. There is a recorded rise seen in heterotopic and ectopic pregnancies post in vitro fertilization.5 Every individual case has to be diagnosed and managed based upon clinical signs, symptoms and examinations such as hCG levels, ultrasonography findings which suggest viability of pregnancy, gestational age and the patient’s inclination to retain her fertility. As ultrasonography provisions advance, there is a better likelihood of early diagnosis, which in turn enhances the possibility of management using medicinal non-invasive methods such as with methotrexate or potassium chloride, and with minimally invasive procedures such as hysteroscopy or laparoscopy, or curettage, thereby preserving fertility. A caesarean scar ectopic pregnancy complicates 1 in 2226 pregnancies.6 Studies have shown that incidence and risk of caesarean scar ectopic pregnancy does not correlate to the number of previous caesarean deliveries.7, 8 The aforementioned data indicates that majority of the cases of non-tubal ectopic pregnancies can be managed with methotrexate alone or with combination of minimally invasive procedures.9 These methods have proven efficacy as the first line of management and preserve the fertility of patients. Methotrexate is the primary choice of medical management at doses of 50mg/m2 body surface area when given as a single dose intramuscular. This is followed by repeating beta-hCG of Day 4 and Day 7. Alternate day systemic methotrexate can be given along with folinic acid. There is still some controversy regarding the role of expectant management as it is considered advantageous in asymptomatic patients with confirmed non-viable pregnancy associated with decreasing trends of beta-hCG levels. There is still a risk of ectopic rupture and this should be conveyed and counselled to the patient who should be kept under surveillance with intensive care and monitoring of clinical signs and symptoms of the same. Patients showing uncontrolled vaginal bleeding and who are hemodynamically unstable, or patients with failed medical management need surgical intervention. In patients where methotrexate is contraindicated, or hemodynamic compromise showing signs of rupture such as heavy vaginal bleeding, abdominal pain, tachycardia, hypotension, guarding and rigidity of abdomen, laparoscopic management is preferred. In patients with active pelvic inflammatory disease, methotrexate is avoided as it can flare up. Therefore, the choice of management in such patients would be laparoscopy under sufficient antibiotic coverage. With the advances in ultrasonography aiding in good and early diagnosis and availability of enhanced laparoscopic approaches, laparotomy is losing its edge. Prospective randomized trials have shown the superiority of laparoscopy over laparotomy, showing reduction in bleeding, requirement of analgesia and reducing length and cost of hospital stay. However, reproductive outcomes, including the rates of recurrence of ectopic pregnancy or intrauterine pregnancy, are not significantly different, as per studies.10
Conclusion
There should be a clear protocol for management of non-tubal ectopic pregnancies in hospitals since there is an anticipated rise in the near future because of an increased rate of risk factors. This case series is a summary of different protocols and methods to manage non-tubal ectopic pregnancies which may be potentially life-threatening if left untreated. Furthermore, there may be repeated ectopic pregnancy, infertility, or even uterine ruptures in future pregnancies, thus the patient must be adequately informed about these complications. There should also be attentive surveillance in following pregnancies to gauge scar integrity during pregnancy and labor. There is a variety of options available in management of non-tubal ectopic pregnancy. Early diagnosis, size, duration, type of non-tubal ectopic pregnancy, beta-hCG levels and the want to preserve fertility will aid in determining the correct modality of management.