Introduction
An ectopic pregnancy occurs when a fertilized ovum gets implanted outside normal uterine cavity.1 It is one of the most common causes of extrauterine pregnancy is 1.3-2.4% worldwide2 and in India it is 1-2% 3. Most common site of ectopic pregnancy is fallopian tube (90%) and it can also occur in the cervix, ovary, myometrium, broad ligament, previous caesarean section scar rarely.4 Extra-uterine pregnancy generally presents at 6-9 weeks of gestation.2 Ectopic pregnancy generally presented with history of amenorrhoea, abdominal or pelvic pain with or without bleeding per vagina and even haemorrhagic shock in case of ruptured ectopic pregnancy. To diagnose an ectopic pregnancy clinical suspicion along with Trans-abdominal sonography or Trans-vaginal sonography and serological confirmation of pregnancy is needed.5 In this article three case reports (all were un-booked patients) have been discussed about live ectopic pregnancy which were diagnosed and managed in Bankura Sammilani Medical College and Hospital, Bankura.
Case 1
A 25 years old female, gravida 3, parity 1+1, living issue one with one abortion followed by dilatation and curettage at ten weeks of gestational age during second pregnancy, presented with complaints of diffuse lower abdominal pain and mild bleeding per vagina for two days and vomiting for ten days. There was history of amenorrhoea for three months. Patient was oral contraceptive pills irregularly since her last pregnancy two years back. Urine pregnancy test came positive. There was no history of abortifacient intake or trauma or recent sexual intercourse. On examination, there was mild pallor with tachycardia (pulse rate 106 beats per minute) and blood pressure 110/66 mm Hg. On per abdominal examination mild tenderness was present in the right iliac fossa and hypogastrium region. On per vaginal examination uterus was normal in size and a 3x3 cm2 globular mass felt in right adnexa with right adnexal fullness, tenderness along with cervical motion tenderness and mild bleeding per vagina. On investigation, hemoglobin 8.7gm% with beta-HCG 1,18,327 mIU/ml. Trans-abdominal sonography showed a well defined thick walled sac like structure of 4x3.5 cm2 the right adnexa with live fetus of 12weeks 3 days maturation with CRL(crown rump length) of 5.8cm, mild free fluid present on pouch of Douglas. She was diagnosed with right sided tubal ectopic pregnancy of 12 weeks and planned for emergency laparotomy. During laparotomy an intact gestational sac with live fetus found on right sided fallopian tube and right ovary, left fallopian tube and ovary were healthy.
Right salpingectomy done and nearly 100ml of serosanguinous free fluid found. Peritoneal lavage and intra-abdominal drain given. Patient received one unit packed red blood cell post operatively. Patient was discharged in stable condition six days after surgery.
Case 2
A 36 years old, gravida 3, parity 2+0 (both normal vaginal delivery, last child birth 18 years ago), presented with complaints of bleeding per vagina and pain in the lower abdomen since last 1 week. She had history of amenorrhoea for 2.5 months. She was taking oral contraceptive pills 15 years regularly and irregularly for last 3 years, and she was suffering chronically with white discharge and pelvic inflammatory disease. On examination, pulse rate was 106 beats per minute, Blood pressure was 112/76 mm Hg, mild Pallor was present. There was no history of abortifacient intake or trauma or recent sexual intercourse. Per abdominally there was mild tenderness in left iliac fossa and hypogastrium. On per vaginal examination cervical motion tenderness was present along with left adnexal fullness and tenderness and mild bleeding per vagina. On investigation, hemoglobin 9.0gm%, beta-HCG 80,027mIU/ml. Transvaginal sonography showed bulky uterus, heterogenous with extra-uterine gestational sac noted in left adnexa containing live fetus of 8weeks 4days (CRL of 10.2 mm), left and right ovary healthy, suggestive of ectopic pregnancy. Patient underwent emergency laparotomy and left sided ectopic pregnancy found in the distal part of fallopian tube and bleeding was present from the fimbrial region. Left and right ovary were healthy. Right and left sided hydrosalpinx were present. Left salpingectomy with fimbriectomy along with right sided tubal ligation done.
500 ml of hemoperitoneum was present and it was suctioned out. Peritoneal lavage and intra-peritoneal drain were given. Patient received 1 unit whole blood intra-operatively and she was discharged in stable condition 6 days after surgery. After 1 month during follow up beta-HCG was <5 mIU/ml.
Case 3
A 30 years old, gravida 3, parity 1+1 (LUCS in first pregnancy 8 years ago and second pregnancy was ruptured tubal ectopic pregnancy of left side of 7 weeks gestation which was treated by left salpingectomy 5 years ago), presented with lower abdominal pain for 2 days with amenorrhoea for 2 months. On examination, urine pregnancy test was positive, pulse rate 90/minute, blood pressure 120/76 mm Hg, mild pallor present. Per abdominally, mild tenderness was present in hypogastrium. Per vaginally uterus was mild bulky and there was no cervical motion tenderness or adnexal fullness. On investigation, hemoglobin was 9.8gm%, beta-HCG 12,212 mIU/ml. On trans-vaginal sonography, a 3x2.8x2.6 cm3 thick echogenic round mass with an apparent fetal pole of 11 mm with gestational age of 6weeks 6days with positive cardiac activity present on right cornual region and there was no free fluid in pouch of Douglas.
After discussing the risk is to benefit ratio with the patient and patient party, conservative management was started with Injection Methotrexate 50mg/m2 intra-muscularly as it is a fertility sparing treatment and Methotrexate halts the trophoblastic growth. After 18 hours patient complained of acute abdominal pain with bleeding per vagina. On examination, pulse rate 120 beats per minute, blood pressure 90/56 mm Hg. Per abdominally severe tenderness present in hypogastrium and per vaginally, severe cervical motion tenderness with fullness in pouch of Douglas was present and hemoglobin was 7.8gm% on hemoglobinometer. Emergency laparotomy was done and 3x3 cm2 right cornual ectopic pregnancy found which was ruptured on posterior surface. 1 litre of blood clot was found intra-abdominally. The ectopic pregnancy was removed but due to uncontrolled bleeding from the cornual end, total abdominal hysterectomy was done. Post-operatively pulse rate 120 beats/minute, blood pressure100/56 mm Hg, oxygen saturation 94% on room air and she was shifted to HDU. Patient received 1unit whole blood intra-operatively and total 2unit PRBC was transfused post operatively. After 48 hours she was shifted to septic ward and after 7 days post-operatively she was discharged in stable condition. On 1 month follow up beta-HCG was <2mIU/ml.
Discussion
Ectopic pregnancy causes 75% of maternal death in first trimester and 9-13% of all pregnancy related deaths.6 In majority of cases ectopic pregnancies implant in different sites of fallopian tube, most commonly in the ampulla(70%) followed by isthmus(12%), fimbria (11.1%) and interstitium(2.4%).7
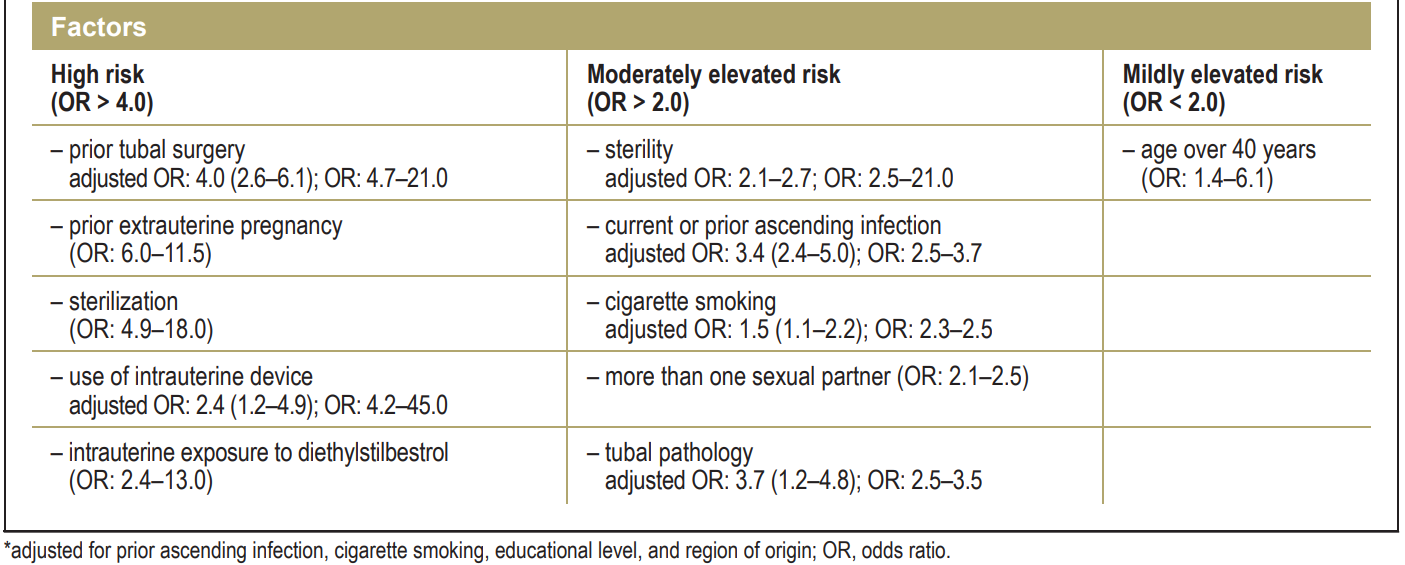
There are many risk factors associated with ectopic pregnancy such as previous ectopic pregnancy, tubal damage or adhesion from pelvic infection or prior abdomino-pelvic surgery, history of infertility, in-vitro fertilization treatment, increased maternal age, smoking. However, there is no identifiable causes in 50% of cases.8, 9
Current use of oral contraceptive pills reduces the risk of unwanted intrauterine pregnancy AOR=0.04(0.02-0.08) and ectopic pregnancy AOR1=0.14(0.07-0.26). However, when contraceptives failed and pregnancy occurred, current use of oral contraceptive pills increase the risk of ectopic pregnancy AOR2=4.08(1.64-10.07) compared with the non-use of contraceptives.10
Tubal pregnancy often becomes symptomatic in the first trimester due to lack of submucosal layer and implantation in the muscular layer of the fallopian tube which allows the proliferating trophoblast to erode the muscular layer. This usually leads to tubal rupture at 7.2 weeks ±2.2.7 Gari R et al. reported a case of live 13 weeks ruptured ectopic pregnancy.11 In case number 1, unruptured tubal ectopic found at 12 weeks 3 day gestation. So, treating clinician should have high suspicion of ectopic pregnancy even beyond early first trimester.
In case number 2, chronic pelvic inflammatory disease was probably the cause of hydrosalpinx and along with this, irregular use of oral contraceptive pills and old age has lead to the ectopic pregnancy.
Cornual ectopic pregnancy (interstitial pregnancy) is rare type of ectopic pregnancy. It comprises 2%-4% of all ectopic pregnancy and 1/2500-1/5000 of all pregnancies.12, 13, 14 The embryo embeds in the funnel shaped junction between uterus and fallopian tube.12 It has high morbidity and mortality (2.2%-2.5%) in the first trimester.13, 15 Without early diagnosis it can grow and causes uterine rupture and bleeding.13, 16
Though cornual resection and hysterectomy is the traditionally accepted surgery, the fertility is affected.12, 15, 16 Successful management includes early ultrasonographic diagnosis, laparoscopic resection and suturing of the uterine cornua.13 Conservative management can be tried by halting the growth and development of the embryo, allowing resorption of the gestational sac17 and for this Methotrexate is used as it arrests the growth of the trophoblasts by inhibiting the DNA synthesis.18 Methotrexate is the most commonly used chemotherapeutic agent for the conservative management of early ectopic pregnancy with a success rate of 91% and upto 66.7% in cornual ectopic pregnancy.12, 17 Meical treatment with methotrexate is less effective when gestational age is >9weeks, beta-HCG >10,000 mIU/ml, fetal cardiac activity is present and when crown-rump length is > 10mm.17, 18
In our case number 3, beta-HCG> 10,000, CRL of 11mm describes the methotrexate failure. After this failure, if patient’s condition was stable, then ideal treatment would be wedge resection of ectopic pregnancy and cornual region of uterus to preserve the uterine integrity.17, 16 But due to hemodynamic instability, hysterectomy was performed.
All these patients were un-booked. The hospital where all these cases were managed, is a tertiary care hospitals and majority of patients who came here are from low socio-economic background and from remote and low resource areas. Health and pregnancy related awarenesses are very limited in those areas and early pregnancy diagnosis and its proper follow up is very difficult to perform. 1st antenatal visit mainly occurs in the late first trimester, in some cases even in the mid second trimester. That’s why the locations of the pregnancies are generally diagnosed lately and early diagnosis of ectopic pregnancies are missed. Ectopic pregnancies are generally diagnosed lately in ruptured form with severe hemoperitoneum and severe hemodynamic instability of the patients.
Conclusions
Ectopic pregnancies are one of the major causes of maternal mortality in first trimester. The rate of this extrauterine pregnancy is increasing day by day due to increased maternal age, smoking, in-vitro fertilization treatment, insufficient knowledge about the proper use of contraceptive pills, increased rate of pelvic inflammatory disease and poor hygiene mainly in the developing countries.
High index of suspicion, early ultrasonography, serum beta-HCG levels help in the early diagnosis of ectopic pregnancy. Unusual mode of presentation of ectopic pregnancy other than tubal rupture and yespresentation beyond early first trimester should be kept in mind when managing a patient of ectopic pregnancy.
Patient’s haemodynamic condition should be assessed thoroughly before deciding the mode of treatment and the decision also depends on the beta-HCG levels, size of the gestational sac and patient’s desire for future fertility. Determining an upper limit of beta-HCG value at which conservative management with Methotrexate can be given is yet to be clear. Appropriate surgical treatment requires advanced laparoscopic skills and techniques to manage or avoid uterine haemorrhage and to reconstruct the cornua in cornual ectopic pregnancy.
Awareness should be spread in remote areas regarding early treatment seeking in case of missed period & irregular menstrual bleeding or spotting, self-identification of signs and symptoms of pregnancy, early 1st antenatal visit, early identification of location of pregnancy by ultrasonography in hospitals. These are possible by educating the ground level workers under rural health mission and arranging health camps more frequently.