Introduction
Fetal growth restriction (FGR) refers to a condition in which a fetus is unable to achieve its genetically determined potential. This functional definition seeks to identify a population of fetuses at risk for modifiable but otherwise poor outcomes. This definition intentionally excludes of fetuses that are small for gestational age (SGA) but are not pathologically small. SGA is defined as growth at the 10th or less percentile for weight of all fetuses at that gestational age. Not all fetuses that are SGA are pathologically growth restricted and, in fact, may be constitutionally small. Similarly, not all fetuses that have not met their genetic growth potential are in less than the 10th percentile for estimated fetal weight (EFW).
Of all fetuses at or below the 10th percentile for growth, only approximately 40% are at high risk of potentially preventable perinatal death. Another 40% of these fetuses are constitutionally small. Because this diagnosis may be made with certainty only in neonates, a significant number of fetuses that are healthy but SGA will be subjected to high-risk protocols and, potentially, iatrogenic prematurity.
For most purposes, an EFW at or below the 10th percentile is used to identify fetuses at risk. Importantly, however, understand that this is not a definitive cutoff for uteroplacental insufficiency. A certain number of fetuses at or below the 10th percentile may be constitutionally small. In these cases, short maternal or paternal height, the neonate's ability to maintain growth along a standardized curve, and a lack of other signs of uteroplacental insufficiency (oligohydramnios, abnormal Doppler findings) can be reassuring to the clinician and parents. Customized growth curves for ethnicity, parental size, and gender are in development so as to improve sensitivity and specificity of diagnosing FGR.
Ultrasound biometry of the fetus is now the gold standard for assessing fetal growth. The measurements most commonly used are the biparietal diameter, head circumference, abdominal circumference and femur length. Percentiles have been established for each of these parameters, and fetal weight can be calculated. The most sensitive indicator of symmetric and asymmetric FGR is the abdominal circumference, which has a sensitivity of over 95 percent if the measurement is below the 2.5th percentile.1, 2 Accurate dating of the pregnancy is essential in the use of any parameter. In the absence of reliable dating, serial scans at two-or three-week intervals must be performed to identify FGR. It should always be remembered that each parameter measured has an error potential of about one week up to 20 gestational weeks, about two weeks from 20 to 36 weeks of gestation, and about three weeks thereafter.
Also useful is the ratio of the head circumference to the abdominal circumference (HC/AC). Between 20 and 36 weeks of gestation, the HC/AC ratio normally drops almost linearly from 1.2 to 1.0. The ratio is normal in the fetus with symmetric growth restriction and elevated in the infant with asymmetric growth restriction. Trans- cerebellar diameter (TCD) is the maximum transverse diameter of the fetal cerebellum. The fetal cerebellar hemispheres are located in the posterior cranial fossa which is resistant to external pressure and growth deviations, thus making it a better indicator for determination of gestational age.3 Conversely, fetal abdominal circumference (AC) is the earliest affected parameter in the process of impaired fetal growth. Thus, a ratio of TCD/AC which is gestational age independent is very useful in predicting FGR. Head circumference is another parameter which remains minimally affected by external pressure effects causing deformation of fetal head and by growth alterations. HC/AC ratio is another gestational age independent parameter which may be used in predicting FGR Many studies have compared the efficacy of several gestational age independent parameters and found that TCD/AC is a better predictor of IUGR. Thus, this prospective comparative study of trans-cerebellar diameter / abdominal circumference versus head circumference / abdominal circumference in predicting intrauterine growth retardation was conducted parameter. In the absence of reliable dating, serial scans at two-or three-week intervals must be performed to identify FGR. It should always be remembered that each parameter measured has an error potential of about one week up to 20 gestational weeks, about two weeks from 20 to 36 weeks of gestation, and about three weeks thereafter.
Aims and Objectives
To compare the efficacy of TCD/AC ratio and HC/AC ratio in detection of FGR.
To prospectively assess the TCD/AC ratio and HC/AC ratio in 200 pregnancies (40 clinically suspected FGR and 160 normal singleton pregnancies.)
To determine the normal value of TCD /AC ratio
Post natal assessment of the newborns to determine
Actual gestational age by new Ballard scoring system and birth weight.
Expected weight for the gestational age according to Fenton’s growth curve.
Compare between 1 & 2 with TCD /AC ratio and HC/AC ratio in prediction of growth restriction.
USG Parameters in diagnosis of FGR
Trans-cerebellar diameter (TCD) is the maximum transverse diameter of the fetal cerebellum. The fetal cerebellar hemispheres are located in the posterior cranial fossa which is resistant to external pressure and growth deviations, thus making it a better indicator for determination of gestational age.3 Conversely, fetal abdominal circumference (AC) is the earliest affected parameter in the process of impaired fetal growth. Thus, a ratio of TCD/AC which is gestational age independent is very useful in predicting FGR. Head circumference is another parameter which remains minimally affected by external pressure effects causing deformation of fetal head and by growth alterations. HC/AC ratio is another gestational age independent parameter which may be used in predicting FGR.
Ultrasound appearance of cerebellum
The fetal cerebellum has a characteristic appearance on ultrasound which changes gradually in shape and echogenicity with advancing gestational age. It has been graded based on its shape as grade I with ‘eyeglass’ (Figure 1 a) at 12–16 weeks, grade II with ‘dumbbell’ (Figure 1 b) at 16 – 28 weeks and grade III with ‘fan’ shape (Figure 1 c) during third trimester and early postnatal life. There is gradual increase in echogenicity from hypoechoic changing to slightly echoic and finally to homogeneously hyperechoic in third trimester.
Cerebellar view
Obtained by rotating the transducer in the axial plane centered on the thalamus to show the cerebellar hemispheres. This view shows the cerebellum, the cisterna magna, the cavum septi-pellucidi and frequently, the anterior horns of the lateral - -ventricles.
Transverse cerebellar diameter (TCD)
TCD is measured by placing calipers on the outer margins of cerebellum visualized in the above -mentioned plane.
Head circumference (HC)
HC is measured on an axial plane traversing thalami and cavum septum pellucidum with the transducer perpendicular to the central axis of the head (Figure 2). The cerebral hemispheres and calvaria should appear symmetric and the cerebellar hemispheres should not be visible on this plane. The ellipse must be drawn with calipers around the outer aspects of the calvarium.
Abdominal circumference (AC)
AC is measured on axial plane containing fetal stomach bubble, umbilical vein and portal sinus (Figure 3). The calipers should be on the skin surface.
TCD/AC ratio
The cerebellum is located in the posterior cranial fossa well protected within the strong bones (petrous temporal and occipital bones) forming it, thus withstanding the extrinsic pressure better than the parietal bones.4 It is relatively resistant to hypoxia due to brain sparing phenomenon leading to maintained blood supply to brain at the cost of systemic supply.5 Abdominal circumference reflects the size of the liver (which correlates with the degree of fetal malnutrition) as well as the volume of subcutaneous plane. Therefore, AC predicts growth restriction more accurately than either BPD or FL.6 However, of the four basic ultrasound measurements the AC generally had the largest reported variability. This is partly attributed to the fact that AC is more acutely affected by growth disturbances than the other basic parameters.7 Hence, a morphometric ratio of TCD/AC can be used to predict asymmetrical FGR.
Materials and Methods
Study population
Prospective comparative cross- sectional study done in 200 pregnant women presented to Malabar Institute of Medical Sciences hospital during March 2018- May 2019. 40 pregnant women in third trimester with clinically suspected FGR, who presented during the period of one year were the study population and 160 normal pregnancies were the controls.
Methods
This was a prospective comparative cross -sectional study with 40 clinically suspecting FGR pregnancies and 160 normal singleton pregnancies over a period of 15 months. Evaluation was done with 3.5 MHz frequency ultrasound. Fetal parameters such as BPD, HC, AC and FL were measured. Data were collected in Excel. Two morphometric ratios- TCD/AC and HC/AC will be calculated. Both TCD/ AC ratio and HC/AC of study group will be compared with that of control group. The values above 2 standard deviations (SD) above mean were taken as FGR and was confirmed by postnatal newborn assessment by modified Ballard score. New born weight is compared with Fenton’s chart. If it is less than 10th percentile for the gestational age, it will be diagnosed as a real case of FGR.
Inclusion criteria
Group 1 (40 cases)
Clinically suspected FGR pregnancies
Singleton, non-anomalous pregnancies
Completed 20 weeks
With a favorable lie to visualize posterior fossa.
Group 2 (160 cases)
Statistical methods
Data were collected in Excel.Data were analyzed using SPSS 21.0. TCD/AC and HC/ AC ratios were calculated. The values were correlated with advancing gestational age to know if these were related to gestational age. Sensitivity, specificity, positive predictive value, negative predictive value and diagnostic accuracy for TCD/ AC and HC/AC ratios in evaluating FGR features were calculated.
Results
This study included total 200 subjects. 160 among them were without FGR (80%) and the remaining 40 were with FGR (20%).
The average age was 28.51 years with standard deviation 4.405. The minimum and maximum age was 19 and 40 years respectively.
In the study of total 200 subjects 83 were primi (41.5%) and 117 subjects were multigravida (58.5%).
Table 2
Summary table for HC/AC and TCD/AC
|
Parameter |
N |
Mean |
Std. Deviation |
Range |
|
TCD / AC |
200 |
1.58 |
0.177 |
1.11; 1.98 |
|
HC / AC |
200 |
1.09 |
0.889 |
0.98; 1.40 |
Mean value for TCD/AC was 1.58 with standard deviation of 0.177. Hence values lying outside the range 1.11; 1.98 were taken as abnormal. In the case of HC/AC ratio, mean value was 1.09 and the standard deviation of 0.889. Hence the normal values lie in the range of 0.98;1.40.
Of the 40 clinically suspecting FGR pregnancies, only 35 had the final diagnosis IUGR based on postnatal assessment. 4 new cases of FGR had been detected among the clinically normal group postnatally. Hence, 39 cases of FGR.
Sensitivity = 89.74%
Specificity = 96.9%
Positive Predictive Value = 87.5%
Negative Predictive Value = 97.5%
While measuring HC/AC values of the subjects, it was found that 40 values had fallen outside the normal range and which suggested FGR by HC/AC method. Post natal assessment revealed that among these 40 patients, only 36 had true FGR and 3 had not. Further 3 more cases were picked up FGR by postnatal method, which were not evident in HC/AC measurement.
Sensitivity = 92.30%
Specificity = 97.51%
Positive Predictive Value = 90%
Negative Predictive Value = 98.12%
TCD/AC value
With TCD/AC measurement, 38 patients had FGR antenatally. Postnatal assessment showed 37. Among these, 38 were had actual FGR and one did not. Further 2 other cases were also picked up for FGR by postnatal assessment.
Sensitivity = 94.87%
Specificity = 99.37%
Positive Predictive Value = 97.36%
Negative Predictive Value = 98.76%
Table 3
Comparison of various parameters of TCD/AC with HC/AC in asymmetrical FGR diagnosis
|
Parameters |
TCD / AC % |
HC / AC % |
Clinical % |
|
Sensitivity |
94.87 |
92.30 |
89.74 |
|
Specificity |
99.37 |
97.51 |
96.9 |
|
PPV |
97.36 |
90 |
87.5 |
|
NPV |
98.76 |
98.12 |
97.5 |
|
Diagnostic Accuracy |
98.50 |
96.50 |
95.50 |
TCD/ AC is showing a sensitivity of 94.87% and specificity of 99.37%. HC/ AC giving a sensitivity of 92.30% and specificity of 97.51%. Diagnostic accuracy of TCD/ AC and HC/ AC are 98.50% and 96.50% respectively. The p-value for TCD/ AC this study is 0.0018 (<0.0001), suggesting that this study is statistically significant.
Table 4
Correlation between FGR response versus Biparietal diameter (BPD) and Femur length (FL)
|
Parameter |
N |
Mean |
Std. Deviation |
Range |
Correlation Coefficient |
value |
|
Biparietal diameter (BPD) |
200 |
8.03 |
0.785 |
6.20; 9.68 |
-0.293 |
<0.05 |
|
Femur Length (FL) |
200 |
6.17 |
0.753 |
4.50; 7.51 |
-0.218 |
<0.05 |
A point-biserial correlation identified a significant negative relationship between Biparietal diameter (BPD) versus FGR response (r=-0.293, p<0.05) and Femur Length (FL) versus FGR response (r=-0.218, p<0.05). This implies that low value of BPD and FL are associated with growth restriction of the fetus.
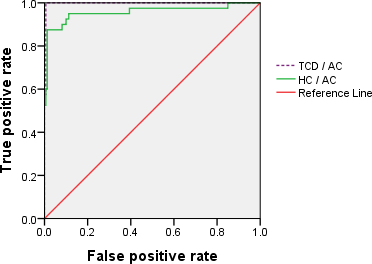
Graphical representation of accuracy of TCD/AC and HC/AC in predicting IUGR
Note: The ROC curve shows the trade-off between sensitivity (or TPR) and specificity (1 – FPR). Classifiers that give curves closer to the top-left corner indicate a better performance. As a baseline, a random classifier is expected to give points lying along the diagonal (FPR = TPR). The closer the curve comes to the 45-degree diagonal of the ROC space, the less accurate the test.
From the figure it is clear that both TCD/AC and HC/AC were good in predicting FGR. Since TCD/AC line is very close to top left corner, which indicates that it is an accurate measure of predicting FGR as compared to HC/AC. ROC curve
Discussion
FGR accounts for a significant increase in perinatal mortality rate as well as immediate neonatal morbidity and continuing long term disability in some of the survivors. TCD/AC which is gestational age independent is very useful in predicting FGR. Maximum number of cases (46.5%) belong to the group 26-30 years. Around 23.5% of the cases belong to the age group 31-35 years, 23% of the cases belong to the age group <= 25 years and 7% of the cases belong to the group >35 years. This study with 200 subjects among which 40 had FGR. 83 were first time mothers, (41.5%) and 117 subjects were multigravida (58.5%).
Clinical assessment
This accounts for a sensitivity of 89.74%, Specificity of 96.9%, positive predictive value of 87.5% and negative predictive value of 97.5%. The overall diagnostic accuracy is 95.50. Diagnostic accuracy is 96.50.The sensitivity for TCD/ AC ratio is 94.87%. Specificity is 99.37%, positive predictive value is 97.36% and negative predictive value is 98.76%. The overall diagnostic accuracy is 98.50.
Bhimarao et al.8 conducted research on efficacy of trans-cerebellar diameter / abdominal circumference versus head circumference / abdominal circumference in predicting asymmetric intrauterine growth retardation had sensitivity, specificity, PPV, NPV & DA (Diagnostic Accuracy) 88%, 93.5%, 77.1%, 96.3% & 92.4% respectively for TCD/AC ratio versus 84%, 92%, 72.4%, 95.8% & 90.4% respectively for HC/AC ratio in predicting FGR. Both the ratios were gestational age independent and can be used in detecting FGR with good diagnostic accuracy. However, TCD/AC ratio had a better diagnostic validity and accuracy compared to HC/AC ratio in predicting asymmetric IUGR. Mourya S et al9 done an evaluation of transverse cerebellar diameter to abdominal circumference ratio in prediction of intrauterine growth retardation. The prevalence of FGR among the study group was 51.5%. The best cut-off of the TCD/AC ratio for predicting growth restriction was 15.87%, giving the sensitivity, specificity, PPV and NPV of 81.25%, 62.25%, 89.65% and 45.45% respectively. Sonographic fetal TCD/AC ratio taken as a gestational age independent, useful, feasible, sensitive method for antenatal diagnosis of FGR, especially in pregnancy with uncertain gestational age is supported by Chavez MR, et al.10 also.
Vinkesteijn AS,5 et al., conducted a retrospective cross-sectional study to establish the increase in fetal transverse cerebellar diameter (TCD) relative to gestational age during normal and restricted fetal growth opining that, in the normally developing fetus the TCD increases with advancing gestational age. Increased TCD/AC values are suspicious of fetal growth restriction. The perinatal mortality in growth restricted fetuses with a small cerebellum was increased two fold over that of other parameters supported by Meyer WJ, et al. Campbell WA,11 et al, conducted a prospective study to evaluate the ability of the transverse cerebellar diameter/abdominal circumference ratio to identify growth retarded fetuses and noted that the transverse cerebellar diameter/abdominal circumference ratio identified growth retardation with a sensitivity of 71%, specificity of 77%, PPV of 79% and NPV of 68%. 14 growth retarded fetuses were missed by the ratio; however, 57% of the missed cases were severely growth retarded. They highlighted that the transverse cerebellar diameter/abdominal circumference ratio could be useful for the assessment of fetal growth retardation but may be normal in cases of severe growth retardation. Tongsong T, et al.,12 evaluated the validity of TCD/AC ratio in predicting IUGR by a prospective descriptive analysis of 167 pregnancies with FGR. The prevalence of FGR was 51.5%. The best cut off value of the TCD/AC ratio for predicting IUGR was 15.4%, giving the sensitivity, specificity, PPV and NPV of 73.26%, 80.25%, 79.75% and 73.86% respectively Sonographic fetal TCD/AC ratio is a gestational age independent method and can be helpful in antenatal diagnosis of IUGR, especially in pregnancy with uncertain gestational age. Agrawal C, et al.,13 and Dilmen G, et al.14 supported these results. In a similar study by Haller H et al.,15 on fetal transverse cerebellar diameter/abdominal circumference ratio in assessing fetal size, TCD/AC ratio was established as a gestational age independent method which could improve diagnostic sensitivity and specificity in the early detection of fetal growth problems.
Conclusion
TCD/AC and HC/AC were gestational age independent parameters and can be used in detecting FGR with good diagnostic accuracy. However, TCD/AC ratio had a better diagnostic validity and accuracy when compared to HC/AC ratio in predicting asymmetric FGR.
Limitations
This hospital based study does not represent an entire population. The Fetal biometry of all these cases were performed by different individuals due to differences in date and time of examination.
Author Contribution
Dr Ambika Premarajan prepared the protocol, collected data, assessed eligibility and methodological quality of studies and wrote the review. Dr Tajunnisa conceived the idea, conducted searches. Dr Saikrishna N assessed eligibility and quality of studies. Dr Ambika performed the statistical analysis and Dr Heera Shenoy T supervised the review.