Introduction
Paraovarian cysts can be a small or large and have been classified based on their presumed origin as paramesonephric, mesothelial or mesonephric.1 Pramesonephric cyst occur most commonly in third o or fourth decades, after the onset o of the functional activity with resultant p secretory product in the tubal type of epithelium.2 These cysts show ciliated and microvillous. cells, similar to oviduct epithelium.2
Case Report
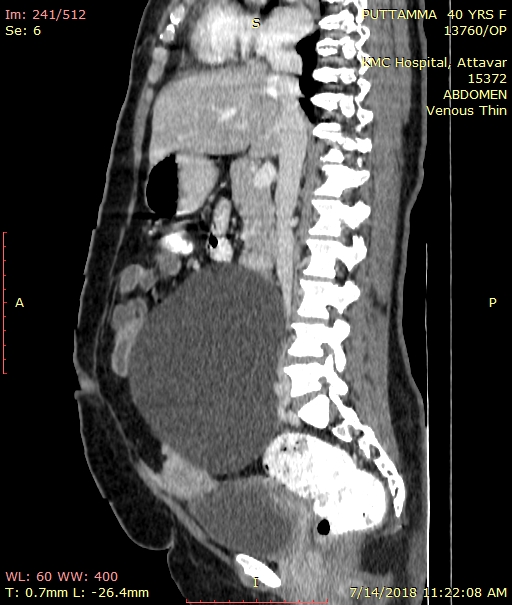
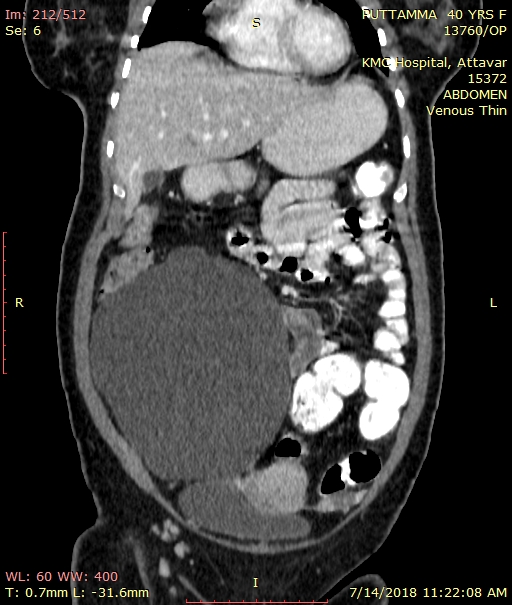
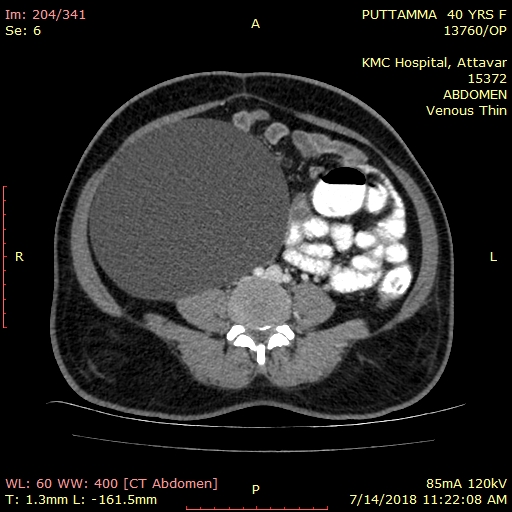
We report a case of paramesonephric duct remnant cyst. A thirty year old P2L2 came with complaints of mass per abdomen since three months. Mass gradually increased in size and not associated with any altered bowel and bladder habits. No history of sudden loss of weight. On examination vitals were stable, mass was about 28 weeks gravid uterus size, cystic in consistency, mobile mass. Per speculum examination showed a healthy cervix and vagina. Bimanual examination- uterus felt separately, fullness of anterior and lateral fornices noted, pouch of douglas appeared free. Her CEA was1.22 and CA-125 was 14. USG showed uterus normal size with ET of 5mm, 14x15 cm abdomino- pelvic cystic lesion noted in right adnexa with no obvious solid component. Right ovary not visualized, features suggestive of right ovarian neoplasm. CECT showed as large abdomino-pelvic cystic lesion of 11x13x16 cam arising from the right adnexa, closely abutting the right ovary medially, extending from the level of upper end plate of L2 till the sacro-coccygeal junction. Anteriorly the lesion is extending upto the anterior abdominal wall. Laterally reaching upto the right lateral pelvic wall. The lesion is abutting and displacing the uterus and small bowel loops medially. Posteriorly, the lesion is abutting the right psoas muscle, infra-renal IVC, right iliac vessels, lower pole of right kidney and recto-sigm oid junction with no evidence of internal septations or enhancing soft tissue densities suggesting benign etiology. Left ovary normal. She underwent laparotomy with intra operative findings being uterus adherent to rectus muscle. Minimal amount of ascites noted and sent for fluid cytology. 15x15 cm paraovarian mass in right side noted and cystectomy done and sent for HPE. Omental biopsy sent for HPE. Fluid cytology came negative for malignant cells. HPE of the cyst came as 1.4 kgs, 15x10x8 cm size which is unilocular, thin walled paramesonephric duct remnant cyst.
Discussion
Paramesonephric duct cysts are the remnants caudal end of the fused paramesophric ducts. The prevalence of these cysts is reported to be 1-5% but symptoma tic presentation is very rare. 2 Preoperatively these cysts should be identified separately from ovarian cyst by visualizing ipsilateral ovary separate from mass which helps us to rule out ovarian pathology. Though these cysts are rarely symptomatic, complications can occur such as internal hemorrhage, torsion, rupture, serous papillary neoplasm. Paramesonephric duct cyst with normal and healthy fallopian tubes has been very rarely reported in literature. A decisive preoperative diagnosis is hardly possible even at the time of surgery as the true a nature of the mullarian cysts s may be difficult to determine by gross appearance as they can be multilocular, adherent to adjacent organs.3 Reported by Lei et al an incidental finding of right adnexal mass on pelvic ultrasonography thought to be ovarian cyst and on laparoscopy a cystic pedunculated mass arising from the right uterine wall anteriorly was seen and HPE showed benign paramesonephric duct cyst remnant. A identical case like ours was reported by Datti et al where the patient had undergone exploratory laparotomy in view of large ovarian mass but on HPE it was paramesonephric duct remnant cyst.
Conclusion
It is very difficult to diagnose paramesonephric duct remnant cyst preoperatively. The importance in reporting this case and citing other reported cases is to bring forward that the rare entities should also be the possible differential diagnosis when looking into a case of paraovarian cysts. If such benign cysts are identified preoperatively patient can have better compliance with laparoscopic surgeries than undergoing exploratory laparotomy.