- Visibility 26 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijogr.2020.092
-
CrossMark
- Citation
An unusual case report of bladder perforation after intrauterine device insertion: Diagnosis and retrieval by flexible hysterofibroscopy
- Author Details:
-
Aditi Rai *
-
Deepak Bolbandi
Introduction
Intrauterine contraceptive device (IUCD) is a long acting reversible contraception method. In all over the world approximately 128 million women are using the IUCD.[1] Uterine perforation is one of the major complications of IUCD. Patient will be asymptomatic for a longer time so early diagnosis is difficult. Risk of abdominal inflammatory response leading to adhesions or perforation of surrounding organs after IUCD perforation.[1] The incidence of uterine perforation by IUCD ranged from 0.4 to 1.6 per 1000 insertions.[2] In 1930 Murphy and Andrews was discovered first case of uterine perforation by IUCD. We hereby describe a case report of a 36-year-old lady who presented with abdominal pain and her imaging with an ultrasound revealed a perforation of the uterus and partially migrated to the urinary bladder lumen.
Case Report
A 36-year-old woman who was para two live two (P2L2) was admitted to our hospital with complaint of lower abdominal pain since 3 hours. Pain was on and off, dull aching in type, not related to activity and was not relieved after taking analgesics. There was no complaints of bleeding per vagina and hematuria symptoms. Her menstrual cycles were regular with normal blood flow. Her last menstrual period was about 5 days prior to presentation. Her past medical history was not significant for any medical comorbidities. She had both cesarean deliveries in, 2010 and 2013. She inserted Cu T IUCD in 2013. Patient was not counselled for checking thread in every cycle. She never checked it. She had no complaints after IUCD insertion.
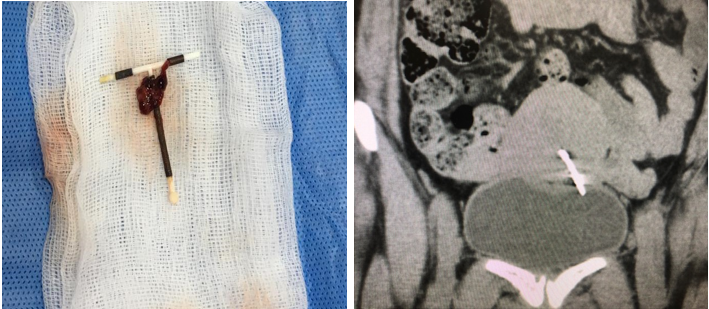
Examination on presentation revealed a young woman in distress. Her pulse rate was 90 bpm, her blood pressure was 110/70 mmHg. Her abdomen was soft and non tender. On admission, bimanual examination was suggestive of normal uterine size. There was no tenderness in either adenexal region. Per speculum examination revealed a normal cervix and vagina with no IUCD thread seen through external os. Relevant investigation was done and found to be normal. The emergency ultrasound scan of her pelvis showed a normal sized, anteverted uterus with low lying IUCD in the lower uterine segment with a horizontal limb seen to penetrate the posterior wall of urinary bladder and tip projecting into lumen. CT scan was done for confirmation, report showed one of horizontal arm is seen perforating the anterior wall of uterus, penetrating the left postero-superior wall of bladder and entering its lumen approximately for a length of 5 mm ([Figure 1]).
Screening cystoscopy was done which showed part of IUCD seen in bladder lumen. Flexible hysteroscopy revealed missing cu T thread where as the vertical arm of the IUD was beyond internal cervical os. The IUCD was easily removed by grasping the tip of the vertical arm with the forceps of the flexible hysterofibroscope and directly pulling it out. The symptoms dramatically improved the day following retrieval. Hemostasis achieved. Foleys catheter was inserted in order to give bladder rest. She received antibiotics, intravenous fluids and analgesics. She was discharged the next day in a stable condition.
Discussion
IUCD is the most effective contraception method world wide. The most common complications are vaginal bleeding, pain and expulsion and rarely IUCD will cause uterine perforation and injury to the adjacent viscera such as appendix, rectum, sigmoid colon and urinary bladder. The presenting features of bladder perforation by IUCD are irritative voiding symptoms, menouria (hematuria during menses). Repetitive and recalcitrant urinary infections and secondary bladder calculus disease.[3] Most authors believe that IUD placement by specialists is very important in preventing perforation, other risk factors are insertion during postpartum period, lactation, low parity, high number of previous abortion.
Mechanism of perforation
Esposito et al[4] postulated that two mechanisms of uterine perforation exist.
Immediate traumatic perforation.
Later “secondary” perforation caused by gradual erosion through the myometrium.
Confirmation of the latter mechanism has been achieved by serial computed tomography (CT) scans performed for nongynecologic purposes.
In the early days of IUDs, insertion instruments were rigid and so perforation was more likely as a consequence.[5] With the Progestasert device, there was documented evidence of a reduction in perforation rate when the inserter was made more flexible and a uterine sound included in the package.[6] Nowadays, insertion tubes are made so that they are more flexible, but not so soft that they buckle easily. Perforation can also happen with a uterine sound. Traditionally, metal sounds were used to measure the uterine cavity length. Plastic sounds are almost certainly safer as they are less rigid. Perforation of the uterus may occur when the uterus is being sounded, or a false track may be created which is then followed by the IUD.
Three anatomical compartments are considered, disregarding the endometrium and serosa. These are as follows:
Uterine cavity.
Myometrium.
Peritoneal cavity.
Partial perforation
A partial perforation may remain as such or it may convert into a complete perforation within a matter of days. This latter conversion is almost certainly due to uterine contractions pushing the device through the myometrium, the force needed depending on the shape of the device.
Complete perforation
With a complete perforation of the uterus, the device may remain near the uterus or it may move within the abdominal cavity. Zakin et al[7] found that the most common location for a completely perforated IUD is the pouch of Douglas. In nearly half of complete perforations, the device is located in the omentum, either loosely or adherent to it; in the latter case it may be so densely adherent that a portion of omentum needs to be excised in order to remove the device. The threads of a completely perforated device will generally not be visible at the cervix by the time of follow-up.
Embedment
Here, a device impinges on the endometrium with a force sufficient to cause pressure necrosis of underlying tissue and penetration into the superficial layers of the myometrium.[8] This phenomenon was seen in the past in women using the Majzlin spring device. When removal of an embedded device is attempted, trauma to tissues may occur. Great care is needed in cases of embedment if marked pain is caused at attempted removal. In one case, this caused a tear which resulted in a 2-liter hemorrhage.[9]
Prevention of uterine perforation
Actions that can help to reduce the risk of uterine perforation associated with insertion of IUDs include:
Avoidance of insertion or taking extra care (with special consent) from 48 hours to 4 weeks postpartum, especially if the woman is breast-feeding.
Use of a plastic rather than a metal sound.
Use of a suitable tenaculum and applying appropriate traction to it.
Provision of less rigid introducers by device manufacturers.
Accurate setting of the flange on the introducer according to the sounding distance and the specific instructions for the device.
A pull-back, rather than a push-out, release mechanism for the device.
Skilled insertion training for clinicians.
Insertion by experienced clinicians.
There is no evidence that use of ultrasound control during the routine insertion of IUDs reduces the risk of perforation occurring. However, complex insertions.
Conclusion
Uterine perforation is a rare complication, but we should explaine to the patient before starting the procedure and prevented if possible by taking all steps to insert devices safely, and diagnosed and managed appropriately. Most cases are due to traumatic perforation that occurs at the time of insertion. However, “secondary” perforation can also occur by gradual erosion. Most of the uterine perforations by IUCD are uncomplicated, with the device lying in a quiescent state in the abdomen. Other organs can be affected, either by direct trauma at the time of insertion or by subsequent erosion. There are higher chances of organ to be affected which is close proximity to the uterus like Bowel and the urinary tract. Most of the cases are “silent” and not recognized at the time of insertion.
Source of Funding
None.
Conflict of Interest
None.
References
- . Family Health International. Netw 2010. [Google Scholar]
- M Harrison-Woolrych, J Ashton, D Coulter. Uterine perforation on intrauterine device insertion: is the incidence higher than previously reported?. Contracept 2003. [Google Scholar]
- P C Ko, Y H Lin, T S Lo. Intrauterine contraceptive device migration to the lower urinary tract: report of 2 cases. J Minim Invasive Gynecol 2011. [Google Scholar]
- J M Esposito, D M Zarou, G S Zarou. A Dalkon Shield imbedded in a myoma: Case report of an unusual displacement of an intrauterine contraceptive device. Am J Obstet Gynecol 1973. [Google Scholar]
- W J Ledger, R Willson. Intrauterine contraceptive devices: the recognition and management of uterine perforations. Obstet Gynecol 1966. [Google Scholar]
- . WHO scientific group. Mechanism of action, safety and efficacy of intrauterine devices. Geneva, Switzerland: World Health Organization. 1987. [Google Scholar]
- D Zakin, W Z Stern, R Rosenblatt. Complete and partial uterine perforation and embedding following insertion of intrauterine devices. I. Classification, complications, mechanism, incidence, and missing string. Obstet Gynecol Surv 1981. [Google Scholar]
- E Wallach, H J Tatum. Clinical Aspects of Intrauterine Contraception: Circumspection 1976*. Fertil Steril 1977. [Google Scholar]
- J A Goldman, D Feldberg, D Dicker. Massive hemoperitoneum due to IUD. Eur J Obstet Gynecol Reprod Biol 1983. [Google Scholar]
