- Visibility 51 Views
- Downloads 11 Downloads
- DOI 10.18231/j.ijogr.2021.118
-
CrossMark
- Citation
Uterine rupture at the fundus during labor: A case report
- Author Details:
-
Sunita Yadav *
-
Susheela Chaudhary
-
Vani Malhotra
Introduction
Uterine rupture is defined as spontaneous tearing of uterus, that may result into fetus expulsion in the abdominal cavity. Rupture uterus is a rare entity with an incidence of 0.07% & often fatal complication with high incidence of fetal & maternal morbidity.[1] It can occur in last trimester or in active labor. The most prevalent cause is dehiscence of previous scar, other factors include trauma, congenital uterine abnormalities, other uterine surgeries like myomectomy, external & internal cephalic version, excessive use of uterotonics, shoulder dystocia.[2]
Rupture of an unscarred gravid uterus is very rare and significantly catastrophic for both mother & fetus, with an estimated occurrence of 1 in 8000 to 1 in 15000 deliveries. Aside cesarean section, irrelevant prostaglandin and oxytocin use, vigorous fundal pressure, previous instrumental abortion & vacuum extraction delivery are the other risk factors for uterine rupture.[3] Shoulder dystocia is one of the most devastating complications of labor that is unpredictable and that’s why unpreventable. In most of the cases, the cause is dystocia from the bony pelvis. The major burden of complications is borne by the fetus. In neglected cases, it result into grave maternal complications like obstructed labor and rupture of uterus. Very rarely, the reverse, uterine rupture leading onto shoulder dystocia can also occur.[4] The present case is reported to emphasize the importance of early recognition of this condition We report a case of uterine rupture in a multiparous laboring patient who presented with shoulder dystocia.
Case Report
A gravida 5 para 2 live 2 abortion 2 with 9 month period of gestation presented to labor room with spontaneous delivery of head 3 hours back, at a private hospital, after being in labour for 8-9 hours. After delivery of head, pain subsided and the trunk failed to deliver. Different manouvers were tried for the delivery of shoulders, but failed. Her previous two deliveries were by normal vaginal delivery 8 years and 5 years back respectively. She had previous two abortions 6 years and 3 years back respectively. Both were spontaneous expulsion followed by dilatation and curettage.
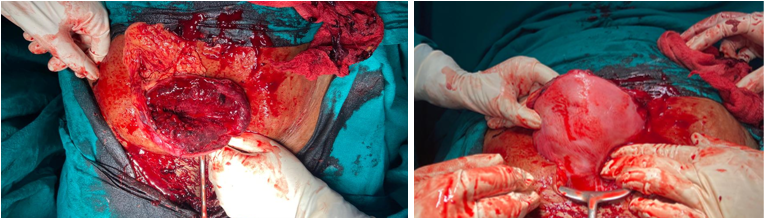

On examination, pulse rate was 140/min. and BP was 100/60 mm Hg. General condition of patient was average. Patient was pale and dehydrated. On per abdominal examination, it was distended and tender, with guarding and rigidity. Uterine contour could not be made out. On local examination, head was lying outside. Turtle neck sign present. Patient was already catheterized, urine was haemmorhagic and was only in tubings. Clinical diagnosis of rupture uterus was made and patient was taken up for laparotomy. Patient was given general anaesthesia. Abdomen was opened vertically, haemoperitoneum of 700ml. Fetal body and limbs along with the placenta was lying in the abdominal cavity and head was in uterus. Baby of 2.34 kg was extracted as breech. A linear rupture of around 10-12 centimeter was present at fundo-posterior region as shown in [Figure 1]. Uterus was repaired in 3 layers and bilateral tubal ligation was done. Abdomen closed in layers. Intraoperatively, 2 PCV and 2FFP and postoperatively 2 PRP were transfused. There was no postoperative complications. Patient charged on post-operative day 10.
Discussion
Shoulder dystocia is defined as difficulty in delivery of shoulders after the delivery of head and it’s incidence is 1in 200. The interval between delivery of head and shoulder should be less than 60 seconds. Usually, anterior shoulder is impacted under pubic symphysis. Rarely, there can occur bilateral impaction, when posterior shoulder also gets impacted over sacral promontory. Shoulder dystocia can lead to birth asphyxia or IUD, brachial plexus palsy, fracture of clavicle or humerus. Many antepartum risk factors like anencephaly, maternal diabetes, macrosomia and intrapartum risk factors like precipitate labor, prolonged duration of labor and forceps delivery have been linked with shoulder dystocia.[5] Yet it is impossible to predict shoulder dystocia. According to a report by the Confidential Enquiries into Stillbirths and Deaths in Infancy, 47% of deaths from shoulder dystocia were within five minutes of delivery of the head.[6] That’s why shoulder dystocia should be promptly managed by a defined protocol, which consists of series of maneuvers that are used consecutively, based on it’s severity.[7]
Seldomly, a forceful uterine contraction can lead to delivery of head, but ruptures the uterus. This results, in expulsion of fetal trunk and shoulders outside the uterus. It fails to deliver shoulders & the trunk. Here, soft tissue of ruptured uterus is causing shoulder dystocia, and not the bony pelvis. Undiagnosed perforation during previous D&C can also cause weakening of uterine wall. Risk factors for uterine rupture include grand multiparity, induction of labor in previously unscarred uterus, uterine anomalies, inappropriate prostaglandin and oxytocin usage, previous instrumental abortion, obstructed labor, vacuum extraction and forceps delivery, vigorous fundal pressure, and intrauterine manipulations.[3] In our patient, the most probable identifiable risk factors were grand multiparity, weakened uterus due to previous D& C and fundal pressure (as told by patient).
Fundal pressure is application of steady pressure on uterine fundus and is considered among the most controversial maneuvers done in second stage of labor. No confirmed benefit of this procedure has been documented but few adverse events have been reported.
In our case scenario, powerful uterine contraction and fundal pressure may have caused giving away of weakened wall at fundus. The shoulders were present high up i.e., above the cervix and not behind the pubic symphysis which suggested rupture of the uterus and shoulder dystocia being the result.
Pan et al. reported a case of uterine rupture due to traumatic fundal pressure in a primigravida woman with an unscarred uterus.[3] Wei et al. also reported similar case associated with assisted fundal pressure leading uterine rupture at 34 weeks of period of gestation in a pregnancy complicated by hydrops fetalis.[8] In a review by Güney et al, 1 out of 8 ruptured unscarred uterus cases was due to fundal pressure.[9] A prospective study comprising of 63 patients with uterine rupture, among them half had a previous scar, concluded that fundal pressure, along with forceps and oxytocin use, was responsible for uterine rupture.[10] In our case, the mother had an unscarred uterus and was not given any prostaglandin or oxytocin during labor as per history. But history of fundal pressure and neglected shoulder dystocia may be the reason of rupture uterus in previously weakened multiparous uterus.
Conclusion
To conclude, Shoulder dystocia is one of the most dreaded complication of labor that is mostly unpredictable and hence unpreventable. Rarely, when such cases are complicated with uterine rupture, it must be recognized early to improve fetal survival rate. Assisted fundal pressure during delivery can result in trauma even in unscarred uterus and leads to traumatic uterine rupture. Early diagnosis is the key to decrease maternal & neonatal morbidity, otherwise both lives could jeopardise.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- PA Martínez-Garza, LP Robles-Landa, M Roca-Cabrera, VJ Visag-Castillo, L Reyes-Espejel, D García-Vivanco. Spontaneous uterine rupture: report of two cases. Cir Cir 2012. [Google Scholar]
- DJ Murphy. Uterine rupture. Curr Opin Obstet Gynecol 2006. [Google Scholar]
- HS Pan, LW Huang, JL Hwang, CY Lee, YL Tsai, WC Cheng. Uterine rupture in an unscarred uterus after application of fundal pressure. J Reprod Med 2002. [Google Scholar]
- V Aditya. Shoulder dystocia, a rare complication of ruptured uterus: a case report and review. Int J Reprod Contracept Obstet Gynecol 2013. [Google Scholar]
- G Dildy, GDV Hankins, SL Clark, FG Cunningham, LC Gilstrap. Shoulder Dystocia. Operative Obstetrics 1995. [Google Scholar]
- . Confidential Enquiries into Stillbirths and Deaths in Infancy. Fifth Annual Report. London: Maternal and Child Health Research Consortium. 1998. [Google Scholar]
- JA O’leary, JA O’Leary. Delivery techniques. Shoulder Dystocia and Birth Injury: Prevention and Treatment 2009. [Google Scholar]
- SC Wei, CP Chen. Uterine rupture due to traumatic assisted fundal pressure. Taiwan J Obstet Gynecol 2006. [Google Scholar]
- M Güney, B Oral, M Ñzsoy, F Demir. Nedbesiz uterus rüptürü: 8 olgunun analizi. Uzmanlik Sonrasi Eğitim ve Güncel Gelismeler Dergisi 2005. [Google Scholar]
- C Vangeenderhuysen, A Souidi. Uterine rupture of pregnant uterus: study of a continuous series of 63 cases at the referral maternity of Niamey (Niger). Med Trop (Mars) 2002. [Google Scholar]
