- Visibility 26 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijogr.2022.033
-
CrossMark
- Citation
Non-ablative Er:YAG laser treatment for stress urinary incontinence (SUI)
- Author Details:
-
Vidya Pancholiya
-
Manish R Pandya *
-
Khushbu K Patel
Introduction
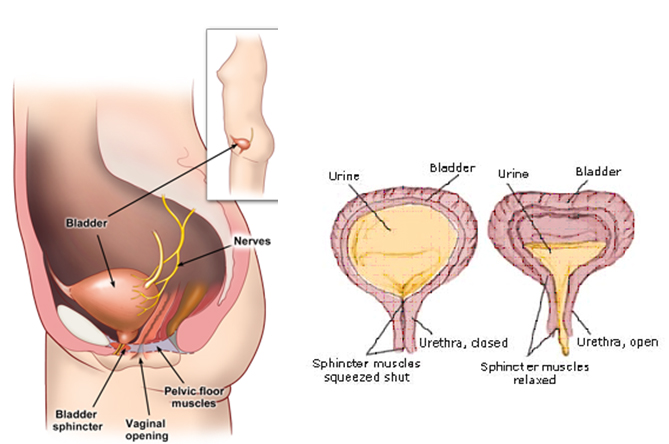
Urinary incontinence (UI) is the involuntary loss of urine, which is objectively demonstrable and with such degree of severity that it is social or hygienic problem is defined by the International Continence Society (ICS).[1] Urinary incontinence is one of the manifestations of the pelvic floor dysfunction.[2] Stress urinary incontinence (SUI) is the most common form of urinary incontinence. SUI is one of the most common seen health problems among the women of a certain age, and is defined as an involuntary urinary leakage during coughing, sneezing, or physical exertion such as sports activities or sudden change in the position.[1], [3], [4]
The exact etiology of the SUI is not completely understood, although the causes of urethral support insufficiency may be a loss of pelvic muscle strength due to damage of pelvic floor innervation after vaginal delivery, altered composition of connective tissue and supporting ligaments due to insufficient and decreased collagen production, or alteration of mucosa due to the menopausal decrease of estrogen and other identifiable risk factors for the condition include pregnancy, cognitive impairment, obesity and advance age.[5], [6] Insufficient support of urethra and bladder or impairment of the urethral sphincter and the reduction of the urethral closure pressure are the anatomical causes of SUI.[7]
Pelvic floor dysfunction (PFD) can lead to pelvic organ prolapse- a condition in which organs, such as uterus, fall or slip out of the original position. In about 15 to 80% of women with PFD, pelvic organ prolapse and Stress urinary incontinence coexists.[8] Among these conditions, one may be mild or asymptomatic, because these conditions are often concurrent. Sometimes, pelvic floor surgery may expose previously asymptomatic conditions; specifically, in previously continent women with pelvic organ prolapse, SUI may develop or worsen after repair of prolapse.[9]
Sometimes due to constipation and vaginal infection, when the muscles of the bladder contract or relax involuntarily there is temporary problem for urinary incontinence. It becomes chronic when there are addition of medical problems like weakened pelvic floor muscles, overactive bladder muscles, etc. Although this is common in women but in some cases due to enlarged prostate men also suffer from this problem. Incontinence can be of different types like functional incontinence, stress incontinence, and urge incontinence, overactive bladder and mixed incontinence.
Initial management of SUI may be done by nonsurgical management, such as weight reduction, hormonal substitution, and physiotherapy, use of pessaries or pelvic floor exercise (e.g. Kegel exercise), etc.[10]
An operative intervention is indicated if above treatments do not lead to improvement within 3-6 months. The tension-free sub urethral slings (TVT- tension-free vaginal tape) were the gold standard for the operative treatment of SUI for the past two decades.[10] It is recommended for moderate to severe cases of SUI preferentially for women after the child-bearing age.
Especially for elder, multi-morbid patients or for recurrent SUI after midurethral sling failure; the trans- or periurethral injection of bulking agents can be an alternative, less invasive treatment option.[11], [12] There are, so far, however, limited treatment alternatives for younger, active women between pregnancies with disturbing incontinence, for example, during physical exercise.
The laser’s medical effects are well established in terms of biochemical, ablative and thermal effects. Especially in moist environment, thermal energy from the laser source, not only effectively enhances collagen structure but also stimulates neocollagenesis. The intermolecular cross-links of the triple helix of collagen shorten, which leads to the immediate tightening of collagen fibrils by two-thirds of their length in comparison to the pre-intervention state as a result of laser irradiation.[13] Currently, minimally invasive intravaginal laser therapy can be the new option for management. There are three different laser modalities have been published for treating SUI, which are as follows: the microablative fractional carbon dioxide (CO2) laser therapy (10,600 nm);[14] dual-phase erbium-doped yttrium aluminium garnet (Er:YAG) laser therapy (2,940 nm) combining fractional cold ablation and thermal ablation,[15] and non-ablative Er:YAG laser therapy (2,940 nm) with SMOOTH mode thechnology.[16], [17] In above all the three cases, laser therapy works by inducing neocollagenesis, thickens and strengthens the anterior vaginal wall, which therefore leads to an improved support of the bladder and the urethra, and consequently, to the continence.[14], [18]
Among all the minimally invasive laser techniques, there is novel laser treatment known as IncontiLase®, which enables collagen remodelling. IncontiLase® is a patent-pending, non-invasive Er: YAG laser therapy. It is used for the treatment of mild and moderate stress urinary incontinence. It is based on non-ablative photo thermal stimulation of collagen neogenesis, shrinking and tightening of vaginal mucosa tissue and collagen-rich endopelvic fascia, and subsequently greater support to the bladder.[19]
IncontiLase® works by following way:
Fotona’s 2.94 µm Er:YAG non-ablative laser with proprietary SMOOTHTM mode technology.
It improves urethral support by photo thermal strengthening of the vaginal wall.
It works on connective tissue in the vaginal mucosa with emphasis on the anterior vaginal wall.
A major advantage of IncontiLase is that the procedure is incisionless. Also it is virtually painless, with no ablation, cutting, bleeding, or sutures. Recovery is extremely quick without need for the use of analgesics or antibiotics.
Two sessions are recommended to alleviate mild or even moderate stress urinary incontinence usually. Special pre-op preparation or post-op precautions are not necessary. Patients can return to their normal everyday activities immediately.
Studies confirm that IncontiLase is an effective, safe and comfortable treatment option in patients with mild and moderate SUI for symptom relief.

Materials and Methods
In this prospective, single-centre study, total 96 patients suffering from stress urinary incontinency underwent treatment with a 2940 nm Er:YAG laser (Fotona) by IncontiLase® Treatment Protocol.
Inclusion criteria
Normal cell cytology (PAP smear)
Negative urine culture
Vaginal canal, introitus and vestibule free of injuries and
Sexual active and non-active women
Exclusion criteria
Pregnancy
Intake of photosensitive drugs
Injury or/and active infection in the treatment area
Undiagnosed vaginal bleeding
Active menstruation
Assessment tools used for this study
KHQ (King‘s health questionnaire)
UDI-6 (Urogenital distress inventory, short form) Questionnaire
3D voiding diary
Satisfaction questionnaire (0-3)
Treatment procedure
IncontiLase® Treatment Protocol with using SClear and MClear speculum
Total duration of Treatment: 20-30 minutes
Step 1
Insertion and initial positioning of the laser speculums SClear and MClear
Insert the G-set SClear or MClear laser speculum into the patient’s vagina to serve as the guide for the laser handpiece with the G-set adapter. After the insertion of the laser speculum into the vaginal canal, rotate it till the single mark is positioned downwards, as shown in [Figure 3].

Insertion and initial positioning of the laser handpiece
When the laser speculum is properly positioned into the patient’s vagina, assemble the laser handpiece PS03 or PS05-9 with the G-set angular (GA) adapter (PS03-GAc or PS05-9GAc). Insert the GA adapter into the laser speculum. Position the mirror of the GA adapter in an upwards direction, as shown in [Figure 4], and align the horizontal scale line of the GA adapter with the far left mark on the laser speculum on upwards position, and push the GA adapter into the laser speculum up to its full length.

Select IncontiLase 1 step on the right hand side and select appropriate handpiece PS03-GAc or PS05-9GAc on the left-hand side. The engraved ring on the handpiece PS03-GAc must be set to 7 mm spot size.

Laser action: angular irradiation of the anterior vaginal wall – first pass
Laser irradiation of the anterior vaginal wall starts from the proximal end of the vaginal canal towards its entrance. With the GA adapter fully inserted and the mirror properly oriented upwards, the practitioner starts delivering laser energy in bursts of six (6) SMOOTH pulses per each location. After the first burst has been delivered, the GA adapter is pulled outwards by 5 mm, as measured by the scale engraved on the GA adapter, and the next burst of 6 SMOOTH pulses is delivered. The burst of 6 pulses is preset as shown on the picture 6 or the practitioner can switch of burst by pressing on the number and then count the pulses by listening to the characteristic soft sound that can be heard each time the laser pulse interacts with the mucosa tissue in the vaginal canal.


Keep repeating the procedure as shown in [Figure 7] until the entrance to the vaginal canal is reached.
When the laser speculum is initially inserted all the way into the vaginal canal, there should be up to 19 activation positions until the exit of the vaginal canal is reached. For shorter vaginal canals, fewer activation locations will be required and thus a smaller number of laser pulses will be delivered.
Laser action: angular irradiation of the anterior vaginal wall – second to sixth pass
After the first pass has been completed, rotate the GA adapter clockwise until its central (longitudinal) marking line is lined up with the next upwards marking on the SClear speculum as shown in [Figure 8]b.
After the GA adapter have been properly positioned for the seconds pass, irradiate the vaginal canal using the same procedure as during the first pass: delivering a burst of 6 SMOOTH pulses every 5 mm of the anterior vaginal wall. Complete this procedure four more times, each time on different marking on the S-clear speculum as shown on [Figure 8].

Step 2
Handpiece exchange
Remove the laser beam delivery system (handpiece PS03 with the GA adapter, PS03-GAc, or similar) from the laser speculum and replace it with the handpiece R11 assembled with the G-set circular (GC) adapter R11-GCc or R11-9GCc.
Insert the GC adapter into the full length of the laser speculum.
Select IncontiLase2 step on the right-hand side and select appropriate handpiece R11-GCc or R11-9GCc on the left-hand side. The engraved ring on the handpiece R11-GCc must be set to 7 mm spot size.

Laser action: circular irradiation of the vaginal wall – first pass
Laser irradiation of the whole vaginal wall starts from the proximal end of the vaginal canal towards its entrance. With the GC adapter fully inserted, the practitioner starts delivering laser energy in bursts of six (6) SMOOTH pulses per each location – as during Step 1. After the first burst has been delivered the GC adapter is pulled outwards by 5 mm, as measured by the scale engraved on the GC adapter, and the next burst of 6 SMOOTH pulses is delivered. The burst of 6 pulses is preset or the practitioner can switch of burst and count the pulses by listening to the characteristic soft sound that can be heard each time the laser pulse interacts with the mucosa tissue in the vaginal canal.

Laser action: circular irradiation of the vaginal wall – second pass
After the completion of the first full circumference pass make one more pass repeating the above described procedure for the first circular irradiation pass.
Step 3
Removal of laser speculum and handpiece exchange
Remove the adapter from the speculum and withdraw the speculum from the vagina. Exchange the R11 handpiece with the PS03 or PS05-9 handpiece equipped with the standard straight adapter.
Laser action: straight irradiation of the vestibule and introitus
Select IncontiLase3 step on the right hand side and select appropriate handpiece PS03 or PS05-9 on the left-hand side. The engraved ring on the handpiece PS03 must be set to 7 mm spot size.

Apply laser pulses on the exposed vestibule, including the urethra meatus, by depositing a patterned laser beam across the whole vestibule and introitus area ([Figure 12]). On each spot location, 2-3 SMOOTH pulses should be delivered before moving to the next spot. Slightly overlap the spots (by approx. 10%). As the urethra orifice is more sensitive, less SMOOTH pulses should be delivered to this area, depending on the patient’s sensitivity. Three full passes across the vestibule and introitus area should be performed.

Depending on the severity of the incontinence, a second treatment after a one month period might be necessary.
Post treatment guidelines
The patient does not require any special after care in the way of medications or special accessories.
It is recommended to respect standard precautions connected with stress urinary incontinence, such as avoiding efforts which may cause pressure to the bladder. This is especially important during the first month after the treatment, i.e. during the period of most intensive neocollagenesis and further collagen remodelling.
It is also recommended that the patient abstain from sexual activities for at least one week after the treatment.
The patient should report and return for check-up at an occurrence of any adverse effects aside from transient mild erythema and edema.
The patient should carry a diary to register changes in incontinence behaviour and any events of leakage.
Repitition
In case the incontinence is still present, a second treatment can be performed one month after the first treatment.
Usually, Two to three sessions are administered in a year followed by a single maintenance session in subsequent year
The measurements were performed before, at 2 months (FU-1) and at 9 months (FU-2).
IncontiLase® Treatment Protocol with G-Runner Robotic scanner
Total Treatment time: 20-30 minutes
Step 1
Setting laser parameters and the G-runner adapter
G-runner laser treatments can be performed with speculums of two different sizes: the larger GClear30 or smaller GClear25. Choose the speculum which fits better to the size of the vaginal opening and the elasticity of the vaginal walls – the speculum should be in contact with the vaginal walls, but not overstretching them.
Clean and disinfect or sterilize the speculum prior to use. Refer to the Cleaning, Disinfection and Sterilization section in the G-runner Operator Manual.
Note that disinfected single-use speculums can be used in contact only with intact mucous tissue.
Set the laser system to the IncontiLase1 mode and the Top Pixel 30 or Top Pixel 25 handpiece, according to the selected speculum. Use the preset parameters, as presented on the laser system’s touchscreen ([Figure 13]).

Attach the yellow GRA-PY adapter on to the G-runner and insert it into the speculum. Start the forward movement of the G-runner by pressing the forward pointing arrow on the G-runner control panel and wait until the adapter reaches the final position. At this point the G-runner will stop and switch direction automatically.
Moisten the speculum with distilled water and, while it is attached to the G-runner adapter, insert it into the patient’s vagina. Keep the orientation of the G-runner in the upright position (control panel up).
Position the speculum so that the observing groove is in the upright position.

|
Incontilase Procedure Step 1 |
||
|
User Interface Mode |
Er: YAG Pulse |
|
|
Hand piece |
G- runner with yellow GRA-PY Adapter |
|
|
Pulse width |
SMOOTH |
|
|
Pulse Number |
4 |
|
|
Frequency |
2 Hz |
|
|
Speculum |
GClear 25 |
GClear30 |
|
Fluence |
10 J/cm2 |
11 J/cm2 |
Laser action: angular treatment of the anterior vaginal wall
Press your foot on the footswitch. This simultaneously initiates laser emission and the G-runner’s rotation. Laser treatment of the anterior vaginal wall starts from the proximal end of the vaginal canal and automatically moves toward the vaginal opening. Laser energy is delivered in bursts of four SMOOTH pulses per each position along the anterior vaginal wall.
Be sure to hold the base of the speculum with one hand and to support the G-runner with your other hand during the treatment. The speculum should not rotate during the treatment.


Proceed with the treatment until the vaginal opening is reached. If at any time the patient shows discomfort, stop the treatment by lifting your foot off the footswitch. Wait for a few seconds before continuing the procedure or decrease the laser fluence. Normally the patient starts feeling discomfort when the scanner reaches the sensitive area one or two centimetres from the vaginal canal opening. At this point it is recommended to stop the laser emission and take out the G-runner adapter by pressing the backward button on the Grunner control board.
Leave the speculum in the vagina while ensuring that it does not accidentally slip out of the vagina during the preparation for the next step.
Step 2
Setting the laser parameters and the G-runner Adapter:
Set the laser system to the IncontiLase2 mode and the ContFull 30 or ContFull 25 handpiece according to the selected speculum. Use the preset parameters as presented on the laser system’s touchscreen ([Figure 5]). Attach the green GRA-FG adapter to the G-runner and insert it into the speculum. Start the forward movement and wait until the adapter reaches the final position. Set the backward direction of G-runner.

Laser action: continuous treatment of the entire vaginal canal – first pass
Press your foot on the footswitch. This simultaneously initiates laser emission and the G-runner’s rotation. Laser treatment starts from the proximal end of the vaginal canal and moves automatically toward the vaginal opening. Laser energy is delivered homogeneously in continuous SMOOTH pulses across the entire vaginal canal.
Be sure to hold the speculum with one hand and support the G-runner with the other hand during the treatment. The speculum should not rotate during the treatment.
Proceed with the treatment until the entrance to the vaginal canal is reached. If at any time the patient shows discomfort, stop the laser by taking your foot off the footswitch. Wait for a few seconds before continuing the procedure or continue after decreasing the laser fluence on the laser system touchscreen. Normally the patient starts feeling discomfort when the scanner reaches the sensitive area one or two centimetres from the vaginal canal opening. At this point it is recommended to stop the laser emission along the first pass and start with the second pass (step 2.3).
|
Incontilase Procedure Step 2 |
||
|
User Interface Mode |
Er: YAG Pulse |
|
|
Handpiece |
G- runner with green GRA-FG Adapter |
|
|
Pulse width |
SMOOTH |
|
|
Frequency |
3.3Hz |
|
|
Speculum |
GClear 25 |
GClear30 |
|
Fluence |
3.5 J/cm2 |
4.5 J/cm2 |
Laser action: continuous treatment of the entire vaginal canal – second pass
Move the GRA-FG adapter to the final position by pressing the forward pointing arrow on the G-runner control panel and wait until the adapter reaches the final position. At this point the G-runner will stop and switch direction automatically.
Press your foot on the laser footswitch and start the treatment as described in the previous section 2.2. Be sure to hold the base of the speculum with one hand and to support the Grunner with your other hand during the treatment. The speculum should not rotate during the treatment.
If you have ended the treatment before reaching the vaginal opening because of discomfort, press the downward arrowhead on the G-runner control panel to remove the adapter from the speculum. Wait for 10 seconds and slowly remove the speculum.

Step 3
Setting laser parameters and the G-runner adapter
Set the laser system to the IncontiLase3 mode and the direct pixel handpiece. Use the preset parameters as presented on the laser system’s touchscreen ([Figure 19]).

|
Incontilase Procedure Step 3 |
|
|
User Interface Mode |
Er: YAG Pulse |
|
Handpiece |
G- runner with green GRA-PG Adapter |
|
Pulse width |
SMOOTH |
|
Frequency |
1.6Hz |
|
Fluence |
10 J/cm2 |
Attach the red GRD-PR adapter to the G-runner. Two red indicator lights should light up and continuously stay lit on the control panel. In this mode, rotation of the G-runner is blocked and it can be used as a manual handpiece.
Apply laser pulses on the exposed vestibule, excluding the urethra meatus; by depositing a patterned laser beam across the whole vestibule and introitus area ([Figure 8]). On each spot location, 2-3 SMOOTH pulses should be delivered before moving to the next spot. Slightly overlap the spots (by approx. 10%). Three full passes across the vestibule and introitus area should be performed.

Post-treatment guidelines
The patient does not require any special after care in the way of medications or special accessories.
It is recommended to respect standard precautions connected with stress urinary incontinence, such as avoiding efforts which may cause pressure to the bladder. This is especially important during the first month after the treatment, the period of most intensive neocollagenesis and further collagen remodelling.
It is also recommended that the patient abstain from sexual activities for at least one week after the treatment.
The patient should report and return for check-up upon any occurrence of adverse effects, aside from transient mild erythema and edema.
The patient should carry a diary to register changes in incontinence behaviour and any events of leakage.
If the incontinence is still present, a second treatment can be performed one month after the first treatment.
Repitition
One month after the first treatment the second treatment is recommended.
Depending on the severity of the incontinence, additional treatment after a one month period might be necessary.
Usually, two to Three sessions are administered in a year followed by a single maintenance session in subsequent years.
Results
A total of 96 (100%) women had stress urinary continence present. They underwent treatment with an Er:YAG (2940 nm) laser in non-ablative fractional mode at Vcare laser centre state of art centre for cosmetic gynaecology, Indore, Madhya Pradesh. The Enrolment of study participants was started in September 2017 and completed in April 2019. An informed consent from the patient is recommended.
The age of the patients ranges from 24 to 70 years of age (average- 47.3 years) and BMI ranges from 19.3-37.2 (average - 25.2). The parity of total women ranges from 1 to 7 (average- 2.5). Here, we excluded nulliparous women. Among 96 women, 83 women were delivered vaginally, 16 were undergone cesarean section and 3 women were delivered by vaginal and cesarean section in subsequent pregnancies. Among 96 women total 86(89.8%) women had vaginal infection among whom 9 (9.4%) women had infection with candiada sp., 43 (44.8%) women had infection with E.coli and 34 (35.4%) had infection with klebsiella.
A total of 96 Patients were treated with IncontiLase protocol, which requires 2-3 sessions with one month interval.
96 patients completed the first session
72 patients completed two sessions
30 patients completed three sessions
Before the treatment, KHQ (King‘s Health Questionnaire); UDI-6 (Urogenital Distress Inventory, Short Form) Questionnaire; 3D Voiding Diary were performed. At 2 months and at 9 months after treatment patients were clinically examined, answered above questionnaires and satisfaction questionnaire for SUI severity and sexual function assessment. A total of 72 patients underwent a 2-month follow-up and 30 patients underwent a 9-month follow-up.
KHQ (King‘s health questionnaire)

KHQ (King‘s health questionnaire) – individual results

[Figure 22] shows individual patient result before treatment and after follow up visits. It shows significant improvement in all 30 patients.
UDI-6 (Urogenital distress inventory, short form) questionnaire
UDI-6 (Urogenital Distress Inventory, Short Form) Questionnaire is the short question form used to assess life quality and symptom distress for urinary incontinence in women.

UDI-6 (Urinary Distress Inventory, Short Form Questionnaire – individual results

3D Voiding Diary
Example of Voiding Diary is given below. Here, we give patients the bladder diary which contains following contents:
Date & time
Liquid intake in ml
Volume of urine passed in ml
Episode of any leakage of urine
Pad change
This simple chart allows patient to record the fluid patient drinks and urine she passes over 3 days (not necessarily consecutive) in the week prior to her clinic appointment. We advised patients to fill this chart and mark with a * if patient has leaked or mark with ‘p’ if patient has needed to change her pad and to write total count.

3D voiding diary

There were no significant differences in fluids intake at observed time points.
3D Voiding Diary – individual results

There were 15 patients reported about the use of pads. All of them significantly reduced the number of pads used which is shown in [Figure 28].

Patients‘ satisfaction questionnaire

Among total of 96 women majority of women (75%) were very satisfied with the treatment and result.
Discussion
The initial management or most patients with SUI, involves a variety of non-invasive interventions, including behavioural therapy and pelvic floor muscle exercises (PFMEs) and for these therapies patience, motivation and time commitment are required. According to the several trials there is demonstrable improvement and satisfactory cure rates in patient adhering to a strict programme of behaviour modification and pelvic floor muscle tonus. However, for successful results, patient compliance and motivation are essential.[6] Other non-surgical treatment options are electric stimulation; vaginal cones, occlusive and intravaginal devices and pharmacological treatments and the reports of the efficacy may vary according to some studies.[20] Bo and colleagues, in a study of 107 patients with SUI, compared the efficacy of electrical stimulation, vaginal cones and a control group and concluded that pelvic floor exercise is superior to both electrical stimulation and vaginal cones in the treatment of genuine SUI in women.[21]
The surgical treatment options are very common, safe and effective option although they are much more invasive, have more complications. It requires a recovery period of several weeks before the patients can return to normal daily activities. [6] Most experts recommend that patients undergo non-surgical options first, as there is insufficient evidence to compare surgery with other interventions.[22] The tension-free sub urethral slings (TVT- tension-free vaginal tape) were the gold standard for the operative treatment of SUI for the past two decades.[10] It is recommended for moderate to severe cases of SUI preferentially for women after the child-bearing age. Especially for elder, multi-morbid patients or for recurrent SUI after midurethral sling failure; the trans- or periurethral injection of bulking agents can be an alternative, less invasive treatment option.[11], [12]
Despite its prevalence and associated distress, embarrassment and diminished quality of life, many women who experience symptoms of SUI choose to delay or do not seek medical treatment because of embarrassment, lack of knowledge about possible treatments or fear that it may require surgical methods.
Following these requirements, the IncontiLase® laser treatment was developed. In our study with 2 and 9 month follow-up of patients with mild-to-moderate stress urinary incontinence treated with non-ablative laser, we demonstrated the efficacy and safety of the procedure. The stress incontinence was measured by KHQ and showed score improvement after IncontiLase® treatment, also at 2 and 9 month follow-ups, indicating significant improvement of SUI.
The indications and contraindications for the use of Er:YAG laser in gynaecology are given below:
|
Indication for use of Er:YAG Laser in Gynaecology |
||
|
Gynaecology indications: |
Genito Urinary indications: |
Cosmetic Indications |
|
Herpes simplex |
Lesions on external genitilia, anus, urethra, scrotum, penis vulva |
Stretch marks |
|
Skin resurfacing ablative and non-ablative |
||
|
Endometrial adhesion |
Polyps and familial polyps of the Colon |
|
|
CIN (Cervical Intraepithelial neoplasia) |
||
|
Skin Rejuvenation |
||
|
Cysts and Condiloma |
||
|
Stress and mixed urinary incontinence (SUI) |
||
|
Treatment of scars – Acne, Post Trauma, Episiotomy |
||
|
Vaginal relaxation syndrome |
||
|
Vulvo Vaginal Atrophy (VVA) |
||
|
Genitourinary Syndrome of Menopause (GSM) |
Treatment of keloids, warts, skin tags |
|
|
Pelvic Organ Prolapse (POP) |
||
|
Breast lifting |
||
|
Lip enhancement and refreshing |
||
|
Cheeks enhancement |
|
Contra-indications (Er:YAG) |
|
|
Urinary tract infection (UTI) |
Collagen, scarring and connective tissue disorders |
|
Injuries or bleeding in areas of tissue to be treated (vestibule and anterior vaginal wall) |
Clotting disorders |
|
Heart or lung disease |
|
|
One of the following urinary tract abnormalities: bladder overcapacity (<300 cc), post void residual >50 cc, spastic bladder, vesicouretral reflux, bladder stones, bladder tumours, ureteral stricture and bladder neck contracture |
Vascular problems (incl. common circulation problems) |
|
Endocrine disorders |
|
|
Hypertension |
|
|
Morbid obesity |
|
|
Abnormal scarring |
Wound healing disorders |
|
Infection or inflammation of treatment area |
Epilepsy |
|
Excessive sun exposure (tanned skin) |
Febrile state |
|
A history of a photosensitivity disorder or use of photosensitizing medication |
Use of iron supplements or an anticoagulant therapy |
|
Pregnancy |
Retin-A and similar products 3 days before and 7 days after treatment |
|
Irradiation in the region of the gonads |
|
|
Diabetes Insulin-dependent diabetes (need a written release from their family physician) |
Accutane (Roaccutane) within 6 months |
|
Systemic antifungal, oral antifungal therapy, or isotretinoin within 6 months |
|
|
Cancer in the area to be treated |
|
|
Autoimmune disorders, such as Lupus |
Use of vasodilators |
|
History of seizures |
Gold therapy An inability to visualize the area to be treated |
|
Herpes simplex infection in the treatment area |
|
|
Anatomic findings not consistent with the diagnosis |
Preoperative histology findings indicative of malignancy |
Regarding the safety and tolerability, we have noticed some adverse effects throughout the whole course of treatment and during the follow-up period like increase in vaginal discharge, slight bleeding, light redness which may persist for few days after treatment. Mild to moderate discomfort or pain during the treatment was noticed in some patients; it was gone as soon as the treatment ended. After the IncontiLase® treatment, all patients returned to their daily activities immediately. The positive effect on the symptoms of SUI was due to neocollagenesis and collagen remodelling. The objective of minimally invasive laser treatment is to achieve selective, heat-induced denaturation of dermal collagen that leads to subsequent new collagen deposition with as little damage to epidermis as possible.[23] Under the influence of specific temperatures from 61ºC to 63ºC, shortening of collagen to longitudinal axis occurs.[13] The processes of collagen remodelling and neocollagenesis starts in addition to the instantaneous collagen and tissue shrinkage reaction[24], [25], [26], [27] and at the end of the processes treated tissue becomes enriched with new collagen and is tighter and more elastic.
The non-ablative Er:YAG laser treatment procedure is easy to learn and does not require specialized surgical skill. This treatment procedure is well tolerated, there is no bleeding, and anaesthesia or hospital are not required. After vaginal Er:YAG treatment, patients are advised to avoid intra-abdominal pressure and sexual intercourse for about 3 days.[28] Vaginal Er:YAG laser treatment offers a minimally invasive alternative treatment option for patients with mild to moderate SUI who do not wish to undergo any invasive procedure or have contraindications to surgery.
Conclusion
The non-ablative Er:YAG laser therapy by IncontiLase® improves the impact of stress urinary incontinence (SUI) symptoms on quality of life and sexual function in premenopausal parous women and provides a promising minimally invasive safe treatment alternative for SUI as per our study results, which, after further optimization, could reduce the need for surgery. It is a fast, simple and well tolerated procedure. It is associated with high level of safety with a short recovery period.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
References
- P Abrams, JG Blaivas, SL Stnton, JT Andersen. The standardization of terminology of lower urinary tract function. The International Continence Society Committee on Standardization of Terminology. Scand J Urol Nephrol Suppl 1988. [Google Scholar]
- RC Blump, PA Nortan. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 1998. [Google Scholar]
- BT Haylen, D Ridder, RM Freeman, SE Swift, B Berghmans, J Lee. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010. [Google Scholar]
- M Cervigini, M Gambacciani. Female urinary stress incontinence. Climacteric 2015. [Google Scholar]
- I Fistonic, SF Gustek, N Fistonic. Minimally invasive laser procedure for early stages of stress urinary incontinence (SUI). J Laser Health Acad 2012. [Google Scholar]
- ES Rovner, AJ Wein. Treatment options for stress urinary incontinence. Rev Urol 2004. [Google Scholar]
- JO Delancey, ER Trowbridge, JM Miller, DM Morgan, K Guire, DE Fenner. Stress urinary incontinence: relative importance of urethral support and urethral closure pressure. J Urol 2008. [Google Scholar]
- SW Bai, MJ Jeon, JY Kim, KA Chung, SK Kim, KH Park. Relationship between stress urinary incontinence and pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 2002. [Google Scholar]
- L Brubaker, GW Cundiff, P Fine, I Nygaard, HE Richter, AG Visco. Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. N Engl J Med 2006. [Google Scholar]
- C Reisenauer, C Muche-Borowski, C Anthuber, D Finas, T Fink, B Gabriel. Interdisciplinary s2e guideline for the diagnosis and treatment of stress urinary incontinence in women :short version- AWMF registry no. 015-005. Geburtshilfe Frauenheilkd 2013. [Google Scholar]
- M Elmelund, ER Sokol, MM Karram, R Dmochowski, N Klarskov. Patient characteristics that may influence the effect of urethral injection therapy for female stress urinary incontinence. J Urol 2019. [Google Scholar]
- I Zivanovic, O Rautenberg, K Lobodasch, G Bünau, C Wasler, V Viereck. Urethral bulking for recurrent stress urinary incontinence after midurethral sling failure. Neurourol Urodyn 2017. [Google Scholar]
- S Thomsen. Pathologic analysis of photothermal and photomechanical effects of laser-tissue interactions. Photochem Photobiol 1991. [Google Scholar]
- P Gonzalez Isaza, K Jaguszewska, JL Cardona, M Lukaszuk. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J 2018. [Google Scholar]
- AR Mothes, M Runnebaum, IB Runnebaum. An innovative dual-phase protocol for pulsed ablative vaginal erbium:YAG laser treatment of Urogynecological symptoms. Eur J Obstet Gynecol Reprod Biool 2018. [Google Scholar]
- N Fistonic, I Fistonic, SF Gustek, IS Turina, I Marton, Z Vizintin. Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women- a pilot study. Lasers Med Sci 2016. [Google Scholar]
- M Lukac, A Gaspar, F Bajd. Dual tissue regeneration: non-ablative resurfacing of soft tissues with FotonaSmoothR mode Er:YAG laser. J laser Health Acad 2018. [Google Scholar]
- GA Lapii, AY Yakovleva, AI Neimark. Structural reorganization of the vaginal mucosa in stress urinary incontinence under conditions of Er:YAG laser treatment. Bull Exp Biol Med 2017. [Google Scholar]
- . . . [Google Scholar]
- PD Wilson, K BO, JH Smith. . Conservative treatment in women 2002. [Google Scholar]
- K Bo, T Talseth, I Holme. single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress continence in women. BMJ 1999. [Google Scholar]
- JM Holroyd-Leduc, SE Straus. Management of urinary incontinence in women: clinical applications. JAMA 2004. [Google Scholar]
- K Kunzi-Rapp, CC Dierickx, B Cambier, M Drosner. Minimally invasive skin rejuvenation with Erbium: YAG laser used in thermal mode. Lasers Surg Med 2006. [Google Scholar]
- DJ Goldberg, JA Samady. Intense pulsed light and Nd;YAG laser non-ablative treatment of facial rhytids. Lasers Surg Med 2001. [Google Scholar]
- B Majaron, SM Srinivas, H Huang, JS Nelson. Deep coagulation of dermal collagen with repetitive Er:YAG laser irradiation. Lasers Surg Med 2000. [Google Scholar]
- B Drnovsek-Olup, M Beltram, J Pizem. Repetitive Er:YAG laser irradiation of human skin: a histological evaluation. Lasers Surg Med 2004. [Google Scholar]
- B Kao, KM Kelly, B Majaron, JS Nelson. Novel model for evaluation of epidermal preservation and dermal collagen remodelling following photo rejuvenation of human skin. Lasers Surg Med 2003. [Google Scholar]
- JI Pardo, VR Sola, AA Morales. Treatment of female stress urinary incontinence with Erbium-YAG laser in non-ablative mode. Eur J Obstet Gynecol Reprod Biol 2016. [Google Scholar]
- Introduction
- Materials and Methods
- Inclusion criteria
- Exclusion criteria
- Assessment tools used for this study
- Treatment procedure
- Step 1
- Insertion and initial positioning of the laser speculums SClear and MClear
- Insertion and initial positioning of the laser handpiece
- Laser action: angular irradiation of the anterior vaginal wall – first pass
- Laser action: angular irradiation of the anterior vaginal wall – second to sixth pass
- Step 2
- Handpiece exchange
- Laser action: circular irradiation of the vaginal wall – first pass
- Laser action: circular irradiation of the vaginal wall – second pass
- Step 3
- Removal of laser speculum and handpiece exchange
- Laser action: straight irradiation of the vestibule and introitus
- Post treatment guidelines
- Repitition
- Step 1
- Setting laser parameters and the G-runner adapter
- Laser action: angular treatment of the anterior vaginal wall
- Step 2
- Setting the laser parameters and the G-runner Adapter:
- Laser action: continuous treatment of the entire vaginal canal – first pass
- Laser action: continuous treatment of the entire vaginal canal – second pass
- Step 3
- Results
- KHQ (King‘s health questionnaire)
- UDI-6 (Urogenital distress inventory, short form) questionnaire
- 3D Voiding Diary
- 3D voiding diary
- Patients‘ satisfaction questionnaire
- Discussion
- Conclusion
- Source of Funding
- Conflict of Interest
