- Visibility 47 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijogr.2022.090
-
CrossMark
- Citation
Cerebroplacental ratio as a predictor of perinatal outcomes in intrauterine growth restriction
Introduction
Intrauterine growth restriction (IUGR) is a condition where the fetus fails to achieve its genetic growth potential and accounts for significant proportion of perinatal morbidity and mortality currently encountered in obstetric practice.[1] IUGR can be defined as sonographically estimated fetal weight <10th percentile for gestational age. A fetus affected by IUGR forms a subset of cases of Small for Gestational Age (SGA) infants.
IUGR can complicate 10% to 15% of all physiologic pregnancies. Growth restricted fetus have a higher incidence of meconium aspiration, still birth, fetal distress leading to caesarean section, birth asphyxia, hypoxic ischemic encephalopathy, pulmonary dysplasia, NICU stay >24hrs, necrotizing enterocolitis, perinatal death etc. Early recognition of such conditions to allow treatment and optimization of both maternal and fetal outcomes is the primary goal of antenatal care4. Gardosi et al[2] demonstrated that there is a significant reduction in the overall stillbirth rate in the setting of diagnosed IUGR where mothers deliver atleast 10 days earlier.
The cerebroplacental ratio is emerging as an important predictor of adverse perinatal outcomes and thus has implications for assessment of well being in IUGR fetuses. The CPR quantifies redistribution of cardiac output by dividing Doppler indices from representative cerebral (MCA) and fetoplacental (UA) vessels.[3] Cerebroplacental ratio most closely reflects acute changes in pO2 and therefore this ratio has been considered superior to the middle cerebral artery pulsatility index (PI) in predicting adverse fetal outcome. Inspite of this, clinical publications related to cerebroplacental ratio are few. In this study we compare the perinatal outcomes[4] of IUGR babies with a normal CPR and an abnormal CPR. Because it is possible to have a normal umbilical Doppler results but an abnormal cerebroplacental ratio, we also look at whether the cerebroplacental ratio improved the prediction of such outcomes.
Materials and Methods
This study was conducted in the Department of obstetrics and gynaecology, Amala Institute of Medical Sciences, Thrissur. This is a prospective study conducted over a period of 18 months from Jan 2018 to June 2019. Antenatal mothers with sonologically detected IUGR and at risk of having an IUGR baby (history of preeclampsia; connective tissue disorders) were included in the study. Antenatal mothers with multiple gestation, diabetes mellitus, history of smoking, anaemia were excluded.
Doppler studies are done for all antenatal women during their third trimester checkups. Ultrasonogram done by a single radiologist was considered. The last doppler measurement before delivery was used to predict perinatal outcome. Doppler parameters like pulsatility index and resistance index of middle cerebral artery and umbilical artery were assessed. Cerebroplacental ratio (CPR) was calculated as ratio of MCA PI/UA PI. A value above or equal to 1.08 is considered normal.
A written consent was obtained from the study subjects. These women were followed up for their remaining Antenatal period irrespective of the outcome. Subjects and babies were followed up till discharge from hospital. For the purpose of analysis, the various parameters studied were divided into maternal, fetal and postnatal variables. Perinatal outcomes are assessed in terms of mean birth weight, meconium staining, caesarean section for distress, apgar score <7 at 5 minutes, birth asphyxia, gestational age <32 weeks at birth, necrotizing enterocolitis, bronchopulmonary dysplasia, hypoxic ischemic encephalopathy, perinatal death.
Data was analysed using Statistical Package for Social Sciences (SPSS) software version 23 and the results were interpreted.
Results
A total of 170 antenatal mothers who met the inclusion criteria were studied. The incidence of IUGR was highest in the age group 21-25 yrs (66%): youngest and oldest being 18 years and 43 years respectively. Most of them were Primi gravidas.
The incidence of abnormal CPR among IUGR babies was 39.4% (67 mothers) among which majority were sonologically detected IUGR.
Mean estimated fetal weight (EFW) according to last ultrasonogram in IUGR babies with an abnormal cerebroplacental ratio was found to be 1797 (± 502) grams. Average period of gestation at the time of birth was 35 weeks and 2 days.
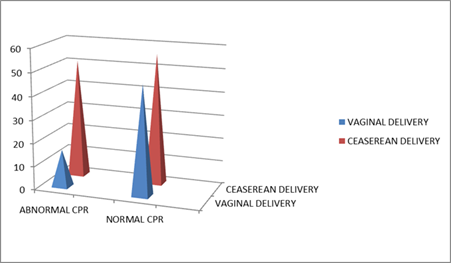
There was a significant increase in the rate of ceaserean section. 107 underwent ceaserean section. 76.12% (51) of fetuses with an abnormal CPR value underwent ceaserean section (45% in normal CPR group).
46 out of 67 babies with abnormal CPR were documented to have birth asphyxia at birth (25 out of 103 in normal CPR group). 64.18%(43) of fetuses with an abnormal CPR value had an APGAR SCORE of <7 at 5mts of life (20% in the normal CPR group).
|
Variable |
Cerebroplacental ratio |
P value |
|
|
Abnormal |
Normal |
||
|
(n=67) |
(n=103) |
||
|
Birth asphyxia (n=71) |
46 |
25 |
0.0001 |
|
Variable |
Cerebroplacental ratio |
P value |
|
|
Abnormal |
Normal |
||
|
(n=67) |
(n=103) |
||
|
APGAR <7 (n=64) |
43 |
21 |
0.0001 |
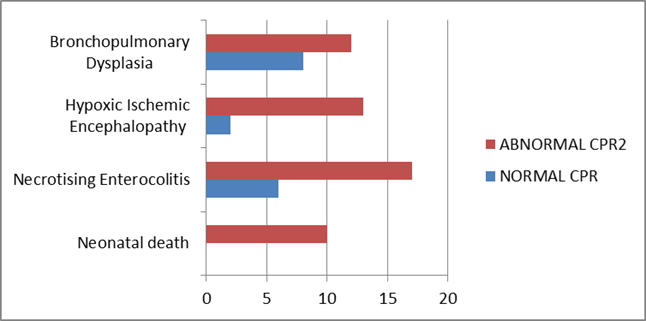
97.02% of babies with an abnormal CPR value had NICU admission majority for fetal distress and IUGR evaluation. Of the total 67 babies with abnormal CPR, 12 babies later developed bronchopulmonary dysplasia (8 in normal CPR group), 13 suffered from HIE (2 in normal CPR group).10 babies with abnormal CPR succumbed to death while there was no deaths in normal group.
Discussion
IUGR is a pathological condition strongly related to the development and function of the uteroplacental and fetoplacental circulations. An adequate fetal circulation is necessary for normal fetal growth. To facilitate this, remarkable changes occur in the maternal, placental and fetal vasculatures. Gramellini et al.[5] calculated the cerebroplacental ratio and found that it remained constant in the last 10 weeks of pregnancy. We, therefore, used a single cut-off value of 1.08 for all cases of 30-41 weeks of gestation. Above this value, Doppler velocimetry was considered normal and, below it, abnormal. Using this cut-off value, we could divide the study population into two groups: Those with a normal ratio and those with an abnormal ratio.
In our study, Incidence of an abnormal cerebroplacental ratio (<1.08) in Doppler studies of the 170 fetuses was found to be 39.4%. Among which most cases were sonologically detected IUGR 34 out of 67 (50.74%) and those complicated with preeclampsia.28 out of 67(41.79%). Several studies have proposed that a combination preeclampsia + IUGR is associated with a phenotype of severe preeclampsia, compared to women with preeclampsia without IUGR.
Cruz-Martinez et al[6] evaluated 210 fetuses at > 37 weeks of gestation suspecting late-onset SGA and reported that an abnormal CPR was associated with a significantly higher rate of emergency cesarean delivery for fetal distress in labor (37.8% vs 20.4%; P < .001) and was a better predictor than an isolated MCA measurement. Figueras et al[7] found that the best predictors for identifying fetuses at risk for emergency cesarean delivery in labor were an abnormally low CPR, an estimated fetal weight less than the third centile, and an elevated PI of the uterine arteries. In our study also we found that there was an increase in the rate of emergency ceaserean rate for fetal distress in fetuses with an abnormal CPR value (76.12% vs 26.88% p= 0.0004).
In our study 64.18%(43) of fetuses with an abnormal CPR value had an APGAR SCORE of <7 at 5mts of life. In fetuses with a normal CPR value only 20.38% (21) had an APGAR OF <7 at 5 mts of life. The incidence was comparable with the studies of Gramellini et al[5] (16.6% vs 2.7%, p<0.001).
In our study, 97.02% (vs 76.6% p<0.0001) of babies with an abnormal CPR value were admitted to NICU. This incidence of comparable with studies of Gramellini et al[5] (77.7% vs 11.1% p<0.001), Flood et al[8] (64% vs 22% p<0.001), Bahado Singh et al. (77.8 vs 41.1% p<0.001).[9]
In our study, the frequency of every category of adverse perinatal outcomes was increased in the group with abnormal CPR values. These differences were statistically highly significant except for meconium staining in amniotic fluid. The results were comparable with the study by Bahado Singh et al.[9] (except for meconium staining and necrotizing enteroccolitis)
In our study, neonatal deaths were more in the group with an abnormal CPR value when compared to those with a normal CPR value (14.9 vs 0 p<0.0001). The incidence was comparable with the results of various studies done by Arias et al,[10] Bahado Singh et al,[9] Flood et al[8] etc.
Conclusion
The cerebroplacental ratio (CPR) is emerging as an important predictor of adverse pregnancy outcome, and this has implications for the assessment of fetal well-being in fetuses diagnosed as intrauterine growth restricted fetus (IUGR). CPR is already decreased when its individual components suffer mild changes and are still within normal ranges. An abnormal ratio is associated with adverse perinatal events. Cerebroplacental ratio should thus be an integral part of Doppler studies in third trimester ultrasound examination.
Source of Funding
None.
Conflict of Interest
None.
References
- DM Walker, N Marlow, L Upstone. The Growth Restriction Intervention Trial: long term outcomes in a randomized trial of timing of delivery in fetal growth restriction. Am J Obstet Gynecol 2011. [Google Scholar]
- J Gardosi, V Madurasinghe, M Williams. Maternal and fetal risk factors for still birth: population based study. BMJ 2013. [Google Scholar] [Crossref]
- SP Chauhan, H Beydoun, E Chang, AT Sandlin, JD Dahlke, E Igwe. Perinatal detection of growth restriction in newborns classified as small for gestational age: correlates and risk of neonatal morbidity. Am J Perinatol 2014. [Google Scholar]
- S Triunfo, F Corvette, E Scazzocchio, M Parra-Saavedra, E Gratacos, F Figueras. Contingent versus routine third trimester screening for late fetal growth restriction. Ultrasound Obstet Gynecol 2016. [Google Scholar]
- D Gramellini, M C Folli, S Raboni, E Vadora, A Merialdi. Cerebral-umbilical Doppler ratio as predictor of adverse perinatal outcome. Obstet Gynecol 1992. [Google Scholar]
- R Cruz-Martinez, F Figueras, E Hernandez Andrade, D Oros, E Gratacos. Fetal brain Doppler to predict cesarean delivery for nonreassuring fetal status in term small-for gestational-age fetuses. Obstet Gynecol 2011. [Google Scholar]
- F Figueras, S Savchev, S Triunfo, F Crovetto, E Gratacos. An integrated model with classification criteria to predict small-for-gestational-age fetuses at risk of adverse perinatal outcome. Ultrasound Obstet Gynecol 2015. [Google Scholar]
- K Flood, J Unterscheider, S Daly, MP Geary, MM Kennelly. The role of brain sparing in the prediction of adverse outcomes in intrauterine growth restriction: results of the multicenter PORTO Study. Am J Obstet Gynecol 2014. [Google Scholar]
- ROB Singh, E Kovanci, A Jeffres, U Oz, O Deren, J Copel. The doppler cerebroplacental RATIO and perinatal outcome in intrauterine growth restriction. Am J Obstet Gynecol 1999. [Google Scholar]
- F Arias. Accuracy of the middle-cerebral- toumbilical-artery resistance index ratio in the prediction of neonatal outcome in patients at high risk for fetal and neonatal complications. Am J Obstet Gynecol 1994. [Google Scholar]
