- Visibility 53 Views
- Downloads 7 Downloads
- DOI 10.18231/j.ijogr.2022.109
-
CrossMark
- Citation
Bimodal approach for a case of cervical ectopic pregnancy
Introduction
Ectopic pregnancy though rare can be a life threatening obstetric emergency. Without prompt diagnosis and treatment, it can lead to significant mortality and morbidity. Cervical Ectopic Pregnancy (CEP) is rare, implantation of pregnancy in endocervical canal and accounts for <1% of all ectopic pregnancies.[1] The only viable treatment option was hysterectomy in the past. However, at present various uterine conservative methods are available which can be life saving and drastically decreases the morbidity associated. CEP Usually presents with vaginal bleeding, which can be profuse and often painless.
Case Description
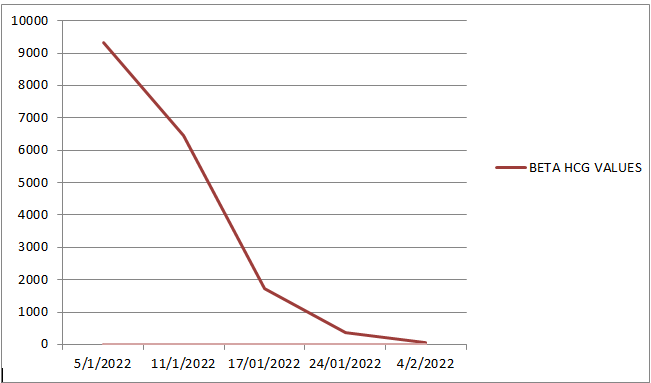
28 years, gravida 3 para1 living 1 abortion 1 (G3P1L1A1) at 12 weeks and 6days of gestational age (GA) with a past history of Cesarean section(CS) and one prior dilatation and curettage (D&C) came to our casualty with complaints of bleeding per vaginum (p/v) on & off for the past month. Patient had a spontaneous conception. Pregnancy was confirmed by a urine pregnancy test (UPT). Early pregnancy scan was suggestive of a single live CEP with thickened endometrium. Serum Beta hCG (βhCG) done following the scan was found to be 9340 IU/ml. 2 doses of Inj. Methotrexate (MTX) was given six days apart at an outside hospital. Patient was monitored with serial transvaginal ultrasound and βhCG values.
|
TVS dated |
Impression |
|
29/12/21 |
A single live CEP with irregular gestational sac (GS) of 2cm |
|
5/1/22 |
A 0.96cm sized cyst with internal echoes seen in the cervix. |
|
11/1/22 |
Clot or retained products of conception noted in the cervical canal associated with ballooning of the cervical canal. |
|
17/1/22 |
Clot or retained products of conception noted at the cervical canal with echogenic contents of 14mm showing peripheral vascularity with distended cervical canal. |
|
4/2/22 |
Clot or retained products of conception noted at the cervical canal with heterogeneous content of size 11.5mm showing peripheral vascularity with distended cervical canal. |
On examination her vitals were stable, no abdominal tenderness. On speculum examination minimal bleeding per vaginum observed, cervix was bulky with an open external cervical os. Per vaginal examination revealed - ballooned out and enlarged cervix with uterus enlarged upto 10 week size and bilateral fornices free. In view of above findings and history of failed medical management, patient was decided for endocervical curettage under anesthesia after obtaining an informed consent regarding the risk of massive hemorrhage, need for blood transfusions, endometritis, need for prolonged hospital stay, possibility of uterine perforation, need for transfer to a tertiary care center with facilities for uterine artery embolisation (UAE), small risk for obstetric hysterectomy in the event of torrential bleeding explained in detail. Following which, after reserving adequate blood products, the patient underwent endocervical curettage(EC) on 11/02/2022. Intraoperatively, using a blunt curette a 4x4 cm mass removed in toto from the cervical canal, suggestive of products of conception. Proceeded with gentle endocervical and endometrial curettage with vigilant monitoring for bleeding and specimens obtained were sent for histopathological examination. Post procedure vitals stable. Patient recovered well, with no further complaints of bleeding and was discharged on post operative day 1.
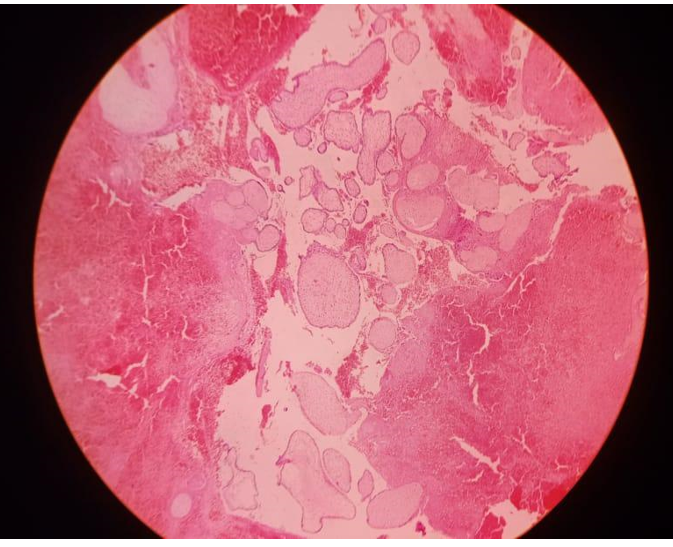
Histopathological Examination (HPE) revealed ([Figure 2], [Figure 3]).

Discussion
CEP is rare and accounts for < 1% of all ectopic pregnancies. Our patient had additional risk factors including previous CS and D&C.[2] As early as 1959 Paalman & Mcelin postulated 5 clinical criteria for diagnosis of CEP. In accordance with which, our patient had a similar presentation with painless vaginal bleeding, ballooned out cervix, cervix enlarged to the size of uterus, an external os which was partially open (internal os closed) and products of conception firmly adherent to the endocervix, satisfying all 5 of Paalman’s criteria.[3] Additionally, with more recent updates published in RCOG, USG diagnosis using TVS has been instrumental in detection of CEP with main diagnostic criteria such as an empty uterine cavity, absence of ‘sliding sign’ and presence of peri-trophoblastic flow on color doppler.[4]
Conservative treatment options for CEP include systemic or local MTX injection, local potassium chloride (KCl) injection or suction and curettage. In patients with uncontrollable hemorrhage, cervical encerclage, balloon tamponade, UAE, uterine artery ligation, in rare cases hysterectomy may be considered.[5]
In the present case, the patient initially was managed with 2 doses of systemic methotrexate. Methotrexate acts by causing disruption of cytotrophoblast syncytialization.[6] Trophoblastic spread, differentiation and invasion was compromised after methotrexate administration.[7] Patient was followed up with serial TVS and serum βhCG. In view of failed medical management, a trial endocervical curettage (EC) was opted for our patient. EC is an established fertility preserving method but results in severe hemorrhage.[8] However, no hemorrhage was observed post procedure in our patient. HPE revealed evidence of attenuation of trophoblastic lining which enabled a controlled and effective curettage without any complications as anticipated with an EC.
Conclusion
Incidence of CEP is increasing due to increased CS rates, increased D&C rates and increased Artificial Reproductive Techniques.[8] Our bimodal approach to CEP, suggests that early diagnosis and treatment with a combined approach can effectively reduce the chances of life threatening hemorrhage and can possibly be one of the safer approaches in the management of a CEP. However, a larger study following the same protocol is required before any conclusion can be established.
Abbreviations
CEP: Cervical ectopic pregnancy; GA: Gestational age; CS: Cesarean section; D&C: Dilation and curettage; P/V: Per vaginum; UPT: Urine pregnancy test; βhCG: Beta human chorionic gonadotropin; MTX: Methotrexate; TVS: Transvaginal ultrasonography; GS: Gestational sac; UAE: Uterine artery embolization; HPE: Histopathological examination; RCOG: Royal college of obstetrics and gynecology; EC: Endometrial Curettage.
Source of Funding
No funding received.
Conflict of Interest
No conflict of interest.
References
- I Marcovici, BA Rosenzweig, AI Brill, M Khan, A Scommegna. Cervical pregnancy: case reports and a current literature review. Obstet Gynecol Surv 1994. [Google Scholar]
- DP Kaur, A Shehgal. Diagnosis and management of cervical ectopic pregnancy - report of three cases. Nepal Med Coll J 2009. [Google Scholar]
- RJ Paalman, TW Mcelin. Cervical pregnancy; review of the literature and presentation of cases. Am J Obstet Gynecol 1959. [Google Scholar]
- CJ Elson, R Salim, N Potdar, M Chetty, JA Ross, EJ Kirk. Diagnosis and management of ectopic pregnancy. BJOG 2016. [Google Scholar]
- O Daniel, GU Rani, PSNRS Sirisha. Cervical Pregnancy: Modes of Management. J South Asian Fed Obstet Gynaecol 2019. [Google Scholar]
- MD Creinin, AM Stewart-Akers, JA DeLoia. Methotrexate effects on trophoblast and the corpus luteum in early pregnancy. Am J Obstet Gynecol 1998. [Google Scholar]
- C Floridon, O Nielsen, C Byrjalsen, B Hølund, G Kerndrup, SG Thomsen. Ectopic pregnancy: histopathology and assessment of cell proliferation with and without methotrexate treatment. Fertil Steril 1996. [Google Scholar]
- S Singh. Diagnosis and management of cervical ectopic pregnancy. J Human Reprod Sci 2013. [Google Scholar]
