- Visibility 88 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijogr.2023.031
-
CrossMark
- Citation
A retrospective study on efficacy and safety of copper T 380 A as a contraceptive method
Introduction
The intrauterine contraceptive device (IUCD) is a safe, effective method for long term use. It is a reversible contraception used all over the world today. They are effective and recommended for use up to 10 years with minimal and tolerable side effects. IUCD in the form of Lippes Loop was introduced in the National Family Welfare Program of the Government of India (GOI) in 1965 and considered as an important spacing method. Cu T 200 B was introduced in the program in 1975. CuT 380A was introduced in 2002, replacing CuT 200B in the program.
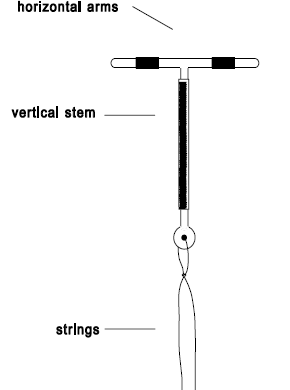
It is a T shaped device made of polyethylene & impregnated with barium sulfate for visibility on X-ray. It is 3.6 cm in length and 3.2 cm in width. There are small copper bands on each horizontal arm of the T, which ensure that copper is released high at the fundus of the uterus. The “vertical stem” is also wound with copper wire. A thin polyethylene string is attached to the bottom of the stem for easy removal. It is available pre packed, with or without a loader.
Copper ions decrease sperm motility and function by altering the uterine and tubal fluid environment, thus preventing sperm from reaching the fallopian tubes and fertilizing the ovum. The device also stimulates foreign body reaction in the endometrium that releases macrophages and prevents implantation.
The advantages of IUCD are that it can be used as an emergency contraceptive if inserted within five days of the first act of unprotected sexual Intercourse. It can be used by lactating women. It does not interact with any medicines. It is effective immediately after insertion and the fertility returns immediately after the removal of IUCD.
Limitation of IUCD is that it does not protect against STDs/ HIV. It is contraindicated in women with active reproductive tract infections (RTIs)/STDs.
The most common indications for removal include desire of pregnancy, sterilization. Some of the side effects include, menstrual irregularities, discomfort, cramps, expulsions, infections, uterine perforations, migration. The method of removal of the device depends on the visibility of the strings during per speculum examination. In IUCD patients with visible strings, removal can be safely done in an outpatient setting. If the strings are not visible, ultrasound is used to locate and aid in the removal of IUCD. Hysteroscopy is a latest option used for IUCD removal under vision.
Aims & Objectives
To determine the efficacy of copper T 380 A as a contraceptive method.
To determine the indications of discontinuation of copper T 380 A.
To identify the difficulties faced during removal in outpatient basis and cases which required removal under anaesthesia in operation theatre.
Materials and Methods
Retrospective analysis on copper T removals done at Gandhi hospital, Secunderabad over 6 months duration, from December 2021 to May 2022. A total number of 128 cases were observed and included in this study.
Results
During this period, a total number of 128 cases of Cu T removals were done. [Table 1] shows the time of insertion. Among 128 cases, Intracesarian insertions were done in 123(96%) cases, Interval insertions were done in 5(3.9%) cases.
[Table 2] shows the age distribution of cases. Majority of these cases belonged to the age group of 20 – 30years (109 cases (85.1%)) and 19(14.8%) cases belong to >30 years of age group.
[Table 3] shows distribution of cases according to parity. 74(57.8%) cases belong to para 1, 50(39%) cases belong to para 2,4(3.1%) cases belong to para 3.
[Table 4] shows the duration of IUCDinsitu. Most of the cases reported after 2-5 years of usage for removal (90(71.8%)), 25(19.5%) cases reported after 1-2 years, 13(10.1%) cases reported after 5 years.
[Table 5] shows the indications for CuT removal. Major indication for removal was desire for pregnancy in 99 cases (77.3%). In 26 (20.3%) cases CuT was removed for sterilization, 1 (0.78%) case for failure of contraception, 1 (0.78%) case for abnormal uterine bleeding and dysmenorrhea, 1 (0.78%) case for uterine perforation. The difficulties faced during removal were non visible strings and missing CuT. Among the removals, as majority of them were inserted during intracesarian period, they were likely to be high up in the uterine fundus with coiled strings and may present with non visible strings. As Gandhi hospital is a tertiary care centre, most cases were referred from periphery in view of non visible strings and difficulty in removal.
[Table 6] shows OPD & OT removals. Out of 128 cases of total Cu T removals, 68 (53.1%) were removed on outpatient basis. Among them, in 52(40.6%) cases, Cu T removal was done by artery forceps after cervical dilatation during menses, and in 16(12.5%) cases, Cu T removal was done under USG guidance. Among the 128 cases, 60 (46.8%) were removed under anesthesia after cervical ripening, out of which 34(26.5%) cases required Shirodkar`s hook for removal, 21 (16.4%) cases required artery forceps and endometrial biopsy (EB) curette, 4(3.1%) cases required hysteroscopy guided removal, 1(0.78%) case required laparoscopic removal due to misplaced IUCD into the abdomen which was embedded in the anterior abdominal wall.

|
Intra caesarian insertion |
Interval insertion |
|
123(96%) |
5(3.9%) |
|
<20 years |
20-30 Years |
>30 Years |
|
0 |
109(85.1%) |
19(14.8%) |
|
P1 |
P2 |
P3 |
|
74(57.8%) |
50(39%) |
4(3.1%) |
|
1-2 Years |
2-5 Years |
>5 Years |
|
25(19.5%) |
90(71.8%) |
13(10.1%) |
|
Desire for pregnancy |
Sterilization |
Failure of contraception |
Uterine bleeding |
Uterine perforation |
|
99(77.3%) |
26(20.3%) |
1(0.78%) |
1(0.78%) |
1(0.78%) |
|
OPD removal |
OT removal |
|
68(53.1%) |
60 (46.8%) |
|
52 (40.6%) – Using artery forceps 16 (12.5%)- USG guidance |
55 (42.9%)- After cervical ripening 4(3.1%) – Under hysteroscopic guidance 1(0.78%)- Laparoscopic removal |
Discussion
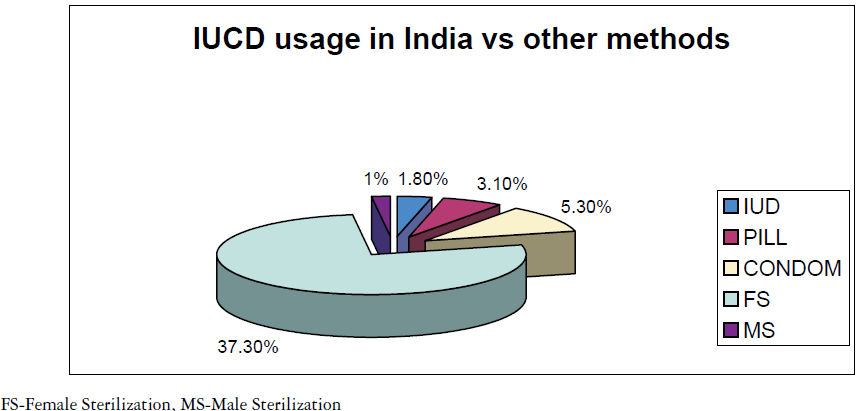
In India only 1.8% of married women of reproductive age use IUCDs. Despite the fact that the government offers IUCD services free of cost, it still remains largely underutilized. One of the main reasons is lack of awareness among the women and associated myths and misconceptions that tend to decrease the acceptance as IUCD as a spacing method. Several investigators have examined the efficacy of various copper IUCD devices. A Cochrane review published by Kulier et al[1] in 2007 made 16 different comparisons of efficacy from the scientific literature. They concluded that the Cu T 380 A was more effective in preventing pregnancy than other devices including multi load 375, multi load 350, Cu T 220, CuT 200. Copper T 380A is approved for 10 years use.
Majority of users belong to the age group of 20 to 30 years with 85.1%, which is similar to the study of Mishra et al.[2] (97.15%). Cu T 380 A allowed many women around the world to avoid unwanted pregnancies and provided effective spacing of pregnancies. Contraception failure rates are less than 1% in many studies. In current study one case presented with pregnancy with IUCD in cervical canal for which Cu T removal was done and continuation of pregnancy was advised. Failure rate in current study is 0.7% which is similar to study done by Sunitha Singal[3] (0.6%), Rwegoshora FJ et al.[4] (0.2%). Copper T 380 A in current study was found to be safe except with some minor problems reported in 3 cases.
An IUCD should be removed at the expiry date, when adverse effects do not resolve, or on patient request. In the present study, the most common reason for discontinuation was desire for pregnancy(99 cases (77.3%)). This is similar to the study in Calabar university[5] where desire for pregnancy was 70.26%, and in study in Jos[6] was 31.9%.
The present study includes all patients consulting for removal of IUCD, and patients referred in view of difficulty in removals like non visible strings and missing IUCD. A multinational study[7] (n=427) that included the United states and European countries, 6.9 per 100 women (6.9%) discontinued IUCD because of pain and menstrual irregularities. It is similar to the present study (1 per 128 women (0.7%)). In another study conducted in Yugoslavia and panama,[8] discontinuation rate was 5 per 100 women (5%). Other reasons for discontinuation include sterilization, abdominal cramps, pregnancy, perforation or migration of IUCD.
Out patient removal is feasible if the strings are visible. Extraction of the IUCD is facilitated by applying controlled traction on the strings during menses. In cases where no strings are visible, possibilities include spontaneous expulsion of the IUCD, curling of the strings in cervical canal, retracted or torn off string, misplacement within the cavity, intramural penetration, or extra uterine migration. Once the IUCD is confirmed to be within the cavity, outpatient removal with use of additional modalities (e.g., Ultrasound guidance, Shirodkar's hook, Endometrial biopsy curette, Artery forceps) can be applied. Curling and retraction of the thread into cervical canal and uterine cavity are major causes of missing strings. Simple pulling of the IUCD with artery forceps and endometrial biopsy curette from uterine cavity was done in 40.6% cases and in 16.4% cases removal was done under sedation after cervical ripening. It is similar to study of Mishra et al.[2]
A sonographic examination is required to identify the location of Cu T. In 12.5% cases Cu T removals were done under USG guidance. Another modality of identifying the location of IUCD is X-ray pelvis with uterine sound. Incidence of missing strings is more common in intra cesarean insertion (79.3%) than interval insertions (3.9%). It is similar to the study done by Mishra et al.[2] As majority of IUCDs were inserted during intra cesarean period, they were likely to be high up in the uterine fundus with curled strings and may present with non visible strings and may be embedded in the uterine endometrium.
If removal is unsuccessful, another attempt may be offered which will be done under anesthesia after cervical ripening with Misoprostol. When this procedure fails, patients are then subjected to hysteroscopy. By Hysteroscopic‑guided removal of IUCD, unnecessary major operation and complications can be avoided. It also offers the advantage of short hospital stay, minimal blood loss, and minimal immediate and late complications. In present study 3.1% cases required hysteroscopic guided removal. Hysteroscopic removal is required in deeply embedded Cu T. Laparoscopic retrieval is done in translocated or migrated IUCD.
Uterine perforation following IUCD insertion is rare and 0.5 to 3 per 1000 insertion are seen according to Mon Lai Cheung et al.[9] Two types of uterine perforation of copper T exists, namely primary and secondary perforations. Both are prone to serious device associated complications. Primary perforation may occur during insertion due to faulty technique, inappropriate timing of insertion, soft uterine wall, wrong measurements of uterocervical length. It typically presents with acute pain abdomen. Secondary perforation is a silent, delayed event occurring due to slow migration of Cu T through uterus due to spontaneous uterine contractions, concurrent bowel peristalsis, bladder contractions. Approximately 80% of IUCD are found in peritoneal cavity after perforation. Migration into surrounding organs is rare but serious complications occur. WHO recommends removing the migrated IUCD as soon as possible. It should be removed even in asymptomatic patients once it has migrated. In case study by Cetinakaya et al.,[10] they found that 23 (41.8%) were located outside the uterine cavity, 3(5.5%) were embedded in myometrium. In current study 1 (0.7%) case presented with migrated IUCD, it is found to be embedded in the anterior abdominal wall with minimal adhesions. Laparoscopic retrieval of the misplaced Cu T was done.
Conclusion
Cu T 380 A is a safe, long-lasting, convenient contraceptive method with very few side effects. The technique of insertion and ease of removal at convenient time makes it an effective and useful contraceptive method. Intracesarean insertion of Cu T can be done easily after counselling the patients. This information may be useful to counsel women who are considering an IUCD and current users who are requesting for removal due to side effects.
Source of Funding
None.
Conflict of Interest
None.
References
- R Kulier, PA O’brien, FM Helmerhorst, M Usher-Patel, C D'Arcangues. Copper containing, framed intra-uterine devices for contraception. Cochrane Database Syst Rev 2007. [Google Scholar] [Crossref]
- N Mishra, N Dalal, V Joshi. Intrauterine Device Insertion during Caesarean Section- A Boon for Rural Women. IOSR J Dent Med Sci 2013. [Google Scholar]
- S Singal, R Bharti, R Dewan, Divya, A Dabral, A Batra. Clinical Outcome of Postplacental Copper T 380A Insertion in Women Delivering by Caesarean Section. J Clin Diagn Res 2014. [Google Scholar]
- FJ Rwegoshora, PS Muganyizi, GF Kimario, GF Kimario. A one-year cohort study of complications, continuation, and failure rates of postpartum TCu380A in Tanzania. Reprod Health 2020. [Google Scholar]
- CU Iklaki, AU Agbakwuru, AE Udo, SE Abeshi. Five-year review of copper T intrauterine device use at the University of Calabar Teaching Hospital, Calabar. Open Access J Contracept 2015. [Google Scholar]
- JT Mutihir, T Iranloye, PFK Uduagbgbamen. How long do women use the intrauterine device in Jos Nigeria?. J Med Trop 2005. [Google Scholar]
- MJ Rosenberg, R Foldesy, DR Mishell, L Speroff, MS Waugh, R Burkman. Performance of the TCu380A and Cu-Fix IUDs in an international randomized trail. Contraception 1996. [Google Scholar]
- CB Champion, B Behlilovic, JM Arosemena, L Randic, LP Cole, LR Wilkens. A three-year evaluation of TCu 380 Ag and multiload Cu 375 intrauterine devices. Contraception 1988. [Google Scholar]
- ML Cheung, S Rezai, JM Jackman, ND Patel, BZ Bernaba, O Hakimian. Retained Intrauterine Device (IUD): Triple Case Report and Review of the Literature. Case Rep Obstet Gynecol 2018. [Google Scholar]
- K Cetinkaya, Y Kumtepe, M Ingec. Minimally invasive approach to cases of lost intra-uterine device: a 7-year experience. Eur J Obstet Gynecol Reprod Biol 2011. [Google Scholar]
