- Visibility 338 Views
- Downloads 41 Downloads
- DOI 10.18231/j.ijogr.2023.080
-
CrossMark
- Citation
Vacuum-assisted caesarean delivery assessment of maternal & fetal outcome
- Author Details:
-
Manisha Agarwal *
-
Sweekrati Solanki
-
Sumedha Sachau
Introduction
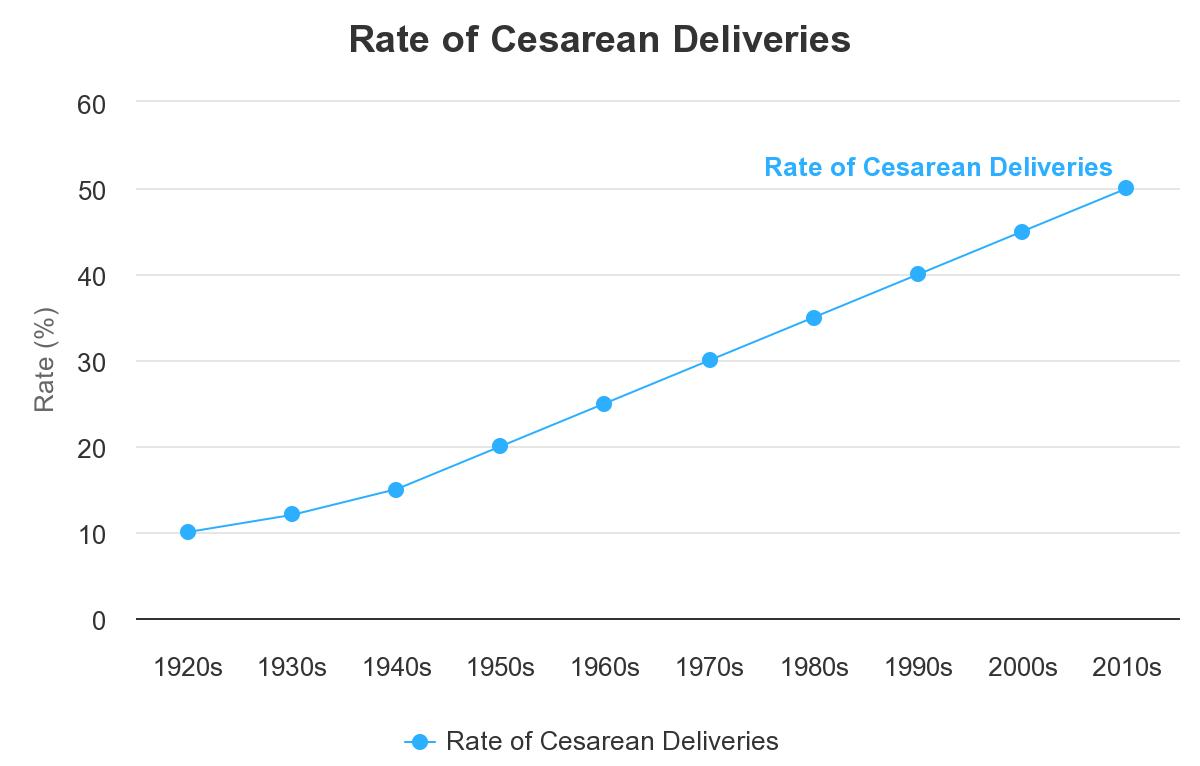
Over the past few decades, there has been a sharp rise in the cesarean delivery rate, which now surpasses 55% in many nations.[1] According to the National Family Health Survey (NFHS-5), India has a C-section rate that is 21.5% greater than the WHO criteria of 15%.[2] Despite public health initiatives to maximize and reduce the use of cesarean sections,[3] the frequency of these deliveries keeps steadily increasing.[4] As a result, doctors will see a greater variety of clinical presentations, which calls for a comprehensive range of delivery alternatives to address various medical situations and enhance outcomes. Vacuum-assisted methods have recently gained popularity for cesarean sections after being largely accepted as a safe and reliable way of surgical vaginal delivery.[5], [6] It can be challenging to make an appropriate incision during an elective cesarean section since the lower uterine segment is frequently not effaced or lengthened by labor. Additionally, the fetal head is not firmly implanted in the pelvis with an elective repeat cesarean surgery.
The use of forceps, fundal pressure, or adding a lateral vertical incision (or "J" incision),internal podalic version, can all be unpleasant for both the woman and the foetus in this situation.[7] The advantages of using a vacuum device in this situation to help with foetal head delivery are listed in the [Figure 1].
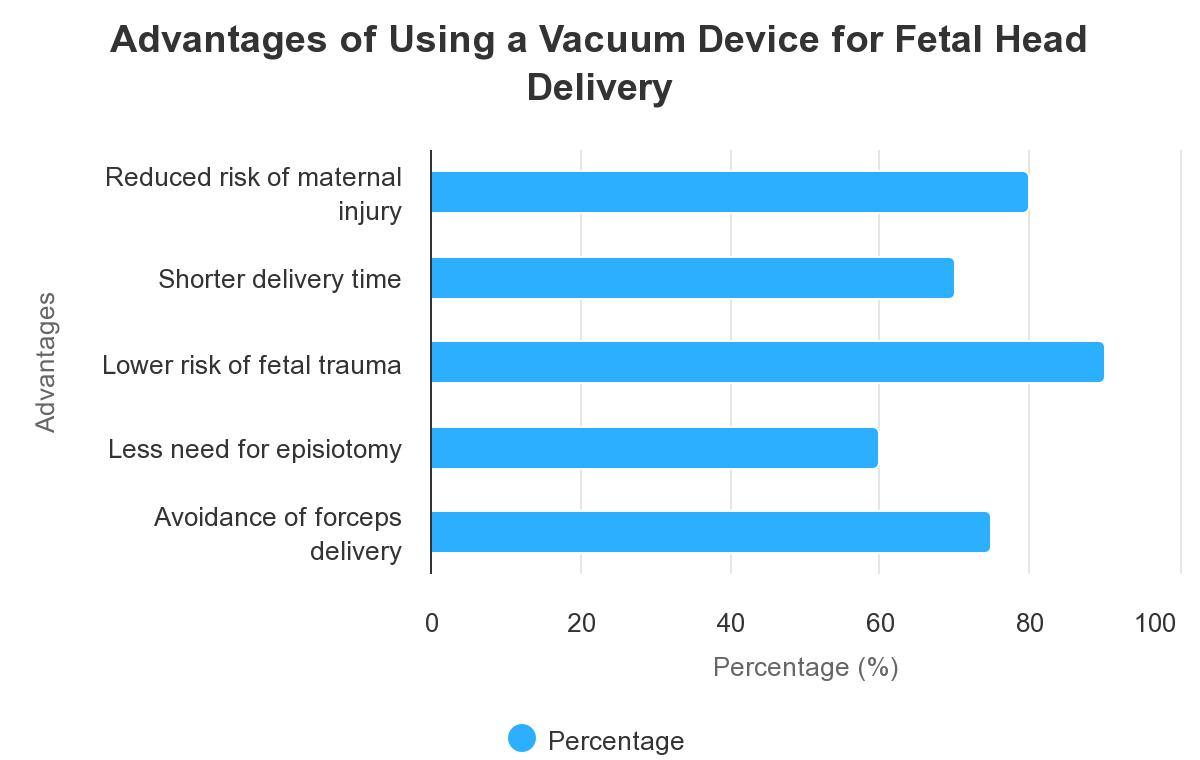
The benefits and safety of routine suction usage during cesarean delivery have not been proven. Several case reports dispute the existence of enhanced results.[8], [9] Although Simonson et al. [10] provide a thorough description of rare incidences of foetal harm linked to vacuum-assisted vaginal delivery, these injuries are uncommon.[11] But using a suction device is a recognized component of obstetric practice. A hospital's piped vacuum supply is frequently employed as a vacuum source. To provide the necessary vacuum for ventouse distribution, we attach it to a pressure reduction valve. In this study, we evaluated the results for the mother and the baby between vacuum-assisted delivery and the standard procedure of manual extraction during cesarean section.
Vacuum extractor history
Due to a variety of factors, including an increase in the number of pregnant women at high risk and the obstetric medical and legal environment, the rate of cesarean deliveries has risen throughout the years. [12]
Depending on the size and positioning of the foetal head, it can occasionally be challenging to deliver a baby during a cesarean surgery. Additionally, it may be linked to excessive maternal problems such as lateral expansions in uterine incisions and cervix-level abrasions. In the aforementioned situations, the use of forceps, increased background pressure with manual extraction, or uterine incisions may help facilitate an easier delivery; nonetheless, these techniques may be unpleasant for both mother and fetus.[13] Recently, there has been an increase in the usage of vacuum cups during cesarean sections to help in fetal head delivery. In 1962, Solomon[14] proposed the use of a vacuum to remove the fetal head; he said that doing so would relieve pressure on the fetus's head, shorten the labor, and lessen fetal hypoxia as well as the size of the incision and vascular damage. James Young Simpson, professor of obstetrics at the University of Edinburgh, created the first effective obstetric vacuum extractor in 1849.
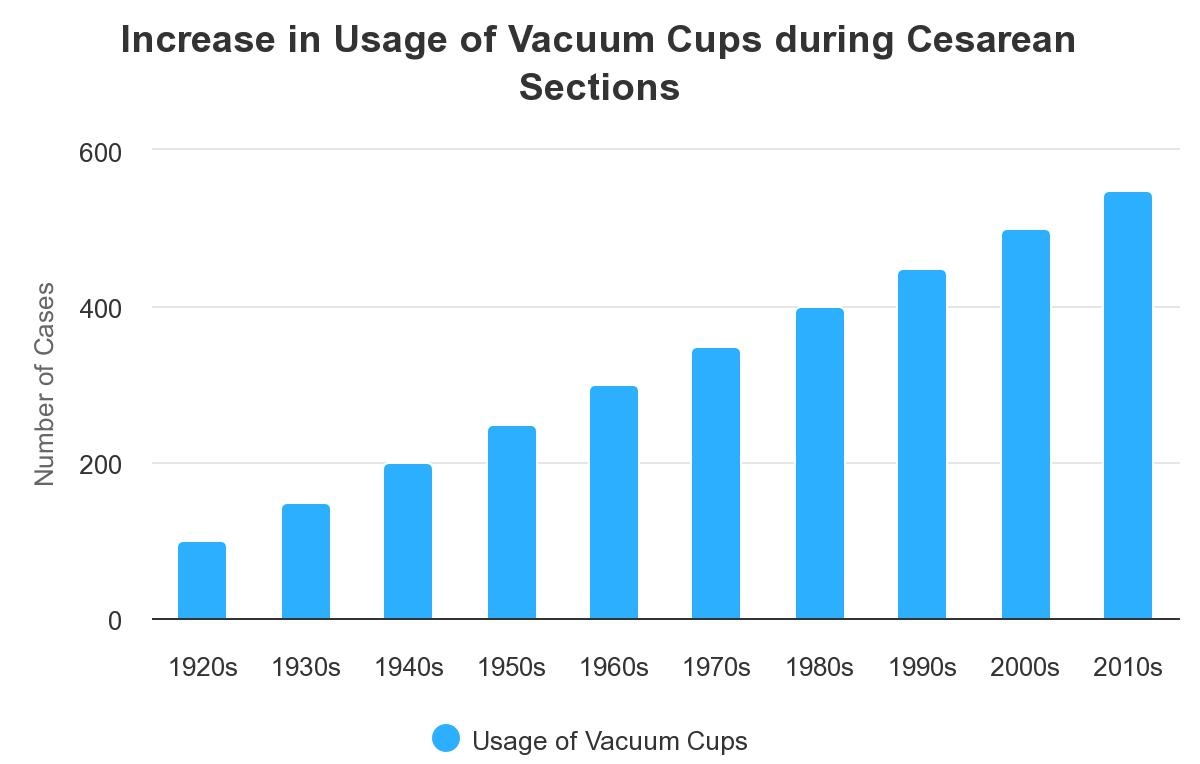
He used a metal syringe that was connected to a soft rubber canister that was put on the fetal head, evacuated, and then traction was applied to the base cup to pull the baby out. The device had various drawbacks, including a lack of pelvic curvature, limited vacuum strength, and the inability to replenish after the first syringe evacuation. Following several breakthroughs, Malmstrom created the metal cup extractor in 1953. Bell-shaped and hemispherical silicone rubber cups have been employed more lately.[15] Because it is simpler to set a metal cup at the occiput-posterior position, more metal cups are successful. Their rigidity, however, can make application challenging and is linked to a higher risk of fetal scalp injury.[16] The soft cup vacuum extractor harms neonates' scalps less than the metal cup does. Some of them include an integrated vacuum relief valve that enables pressure to be attained fast and precisely regulated. These can be used with either a hand vacuum or an electric suction device.[17]
Vacuum-assisted cesarean births can sporadically result in difficulties for both the mother and the fetus. Chignon (iatrogenic caput succedaneum), cephalhematomas, and possibly fatal subgaleal or sub-aponeurotic bleeding are typical neonatal problems. Bruising, laceration and retinal hemorrhages are among the minor side effects.[10] Compared to forceps or cesarean delivery, vacuum extraction has a lower rate of maternal harm. Perineal lacerations, hematomas, blood loss and anemia, urine retention, and chronic issues with fecal and urinary incontinence are just a few of the possible side effects.
Materials and Methods
At Lucknow's Greencross Hospital, a prospective study was carried out between June 2012 and April 2018. The participants in this study were 500 pregnant women. The Institutional Human Ethical Committee authorized this study. Informed consent was obtained after patients were counseled on the potential hazards and advantages of this research methodology. In this cohort study, 250 caesarean sections were carried out in each case with vacuum assistance using a soft cup vacuum extractor on the foetal scalp (diameter: 6 cm) and manual evacuation of the head as usual with fundal compression as support. All of the patients underwent planned caesarean procedures since there was no uterine activity and no amniotic fluid was still present.
[Figure 1] The vacuum system for ventouse delivery is shown. A: hospital-piped vacuum supply was connected to a vacuum cup. The curve of the fetal head and the entire occiput were covered and accommodated. B: A regulator for the vacuum.
Spinal anesthesia was given to all mothers. The following conditions had to be met: singleton gestation, acephalic presentation without fetopelvic engagement on vaginal examination, absence of pregnancy or medical issues, and consent of the patient to be randomly assigned to the delivery method. Pregnant people with obstructed labor or engaged fetal heads, fetal structural malformations, intrauterine fetal deaths, or indications of a high-risk fetal condition were excluded.
The vacuum apparatus employed in our investigation consisted of a vacuum cup that was connected to a vacuum source. The entire occiput and each fetal head shape were uniformly covered and tailored with a soft, silicone obstetric vacuum cup with a diameter of 6 cm. To create the vacuum necessary for ventouse delivery, a hospital's piped-vacuum supply with a vacuum regulator was employed, which required 300 mm Hg (5.5 lb/inch2) of pressure. Compared to the vacuum pressure utilized for an assisted vaginal birth, this vacuum pressure was significantly lower (550-600 mm Hg). Before attaching the vacuum cup to this suction line, the vacuum was calibrated at Full Vacuum (300 mm Hg). The vacuum cup was positioned over the occiput after the membranes were ruptured and the uterine incision. The suction became immediately available when the previously used clamp was removed, and the vacuum cup was fastened to the head. After fifteen to twenty seconds, modest fundal pressure was combined with traction to draw the uterine incision towards the center. To finish the treatment, it was helpful to hold the device close to the vacuum cup's base while applying modest fundal pressure.
The vacuum was turned off and the cup was taken out after the head was delivered. It took only about 100 mm Hg to secure the cup to the embryonic head.
For conventional manual extraction deliveries, if labor did not start after two manual efforts, the delivery could continue utilizing forceps blades, or knives. All deliveries were timed using a stopwatch from the baby head's complete delivery through the fetal membranes herniating through a transected lower uterine segment (amniotomy or herniation).
While the attending pediatrician evaluated the infant's overall status, we recorded the Apgar score[18] at one and five minutes. Each day, before releasing a youngster, they were all carefully examined. Particular focus was placed on the header. A variety of information was gathered, including the mother's age, body mass index (BMI), cephalic delivery method, the time between uterine entry (amniotomy or herniation of fetal membranes through a fully transected lower uterine segment) and cephalic delivery, estimated blood loss for performance, birth weight, neonatal Apgar score, neonatal trauma (including evidence of scalp abrasion, bruising, cephalhematoma, subgale Important maternal and newborn surgical and postoperative data were documented.
Statistical analysis
The data were analyzed using statistical tools. The statistical study used the Studentt-test for continuous data and the Chi-Square test for categorical variables. Counts were provided for categorical variables, whereas mean standard deviation and mean values were reported for continuous data (SD). Statistical significance was defined as a 0.05 p-value.
Results

Total 250 women were assigned to the vacuum extraction group in the randomization process, and 250 to the manual extraction group. Their demographics are presented in [Figure 4] as well. We point out that there was no statistically significant difference between the manual extraction and vacuum extraction groups in terms of mean age, mean parity, or mean birth weight.

[Figure 5] displays post-operative and operational information for the manual and vacuum extraction groups. While the total blood loss was not statistically different between the manual and vacuum extraction groups, there was a significant variation in the length of the uterine incision.

[Figure 6] displays newborn statistics for groups that underwent manual and vacuum extraction. Our findings did not indicate any differences between the two groups of neonates' Apgar scores in the first and fifth minutes. Between the two groups, there were no changes in neonatal resuscitation or SNCU admission.
Discussion
Over the past few decades, the prevalence of cesarean deliveries has rapidly increased over the world, it crosses the threshold of 15% and is now 21.5%.[2] Negative pressure techniques have lately shown clinical efficacy and have gained widespread use for caesarean sections after establishing a safe and reliable way of surgical vaginal delivery. In order to assess the maternal - fetal outcomes, we contrasted the delivery of a free-floating head by vacuum extractor as well as manually during caesarean section. Pelosi and Apuzzio[8] reported the first study on the use of a soft vacuum cup (silastic) for caesarean delivery in 2009. This method successfully delivered 35 neonates without any fetal death, including 20 through elective repeat caesarean sections and 15 during original non-elective caesarean sections. However, because of the high rates of dislocation and general failure, the popularity of the cosmetic soft vacuum cups significantly dropped even if there were no surgical or uterine dilatation issues in their series.[17] Arad et al.[9] examined the neonatal outcomes of 8 patients that delivered by vacuum as well as 10 patients who delivered by manual extraction in a prospective examination of eighteen elective caesarean sections. There were no substantial or statistically significant differences between the groups in terms of birth weight, acid-base status as assessed by cord blood gases. Uterine incision takes more time to completion of delivery in compare to the vacuum group (79.4 vs 40.9 seconds, P<0.01), but the difference was not clinically significant.

The most recent study, a major randomized controlled trial comparing vacuum-assisted delivery (n=90) to manual extraction (n=90) after elective caesarean section, was conducted by Sritippayawan and Chantrapitak.[19] Labor time was significantly reduced in the vacuum group when contrasted to the manually delivery group when a soft cup was used to assist delivery of an unengaged fetal head (86.3±53.9 vs 65.3±31.2 seconds, P<0.01). The Apgar scores were unchanged, and there was no indication of chignon. There was no change in the Apgar scores, and there was no sign of chignon. However, the mean blood loss was marginally higher in the vacuum group (576.7± 182.9 mL vs 504.4± 204.9 mL, P = 0.31). The authors concluded that lengthy fundal compression was not necessary during the rapid, painless, and safe vacuum-assisted caesarean extraction of the fetal head.
The U-D interval in both categories is statistically significant, according to the current study. However, Arads et al.[9] also showed that the woman and fetus have negative effects when the U-D interval (the time between the last uterine incision and full delivery) is prolonged.
Using a vacuum extractor during an elective cesarean delivery result in decreased blood loss during delivery. Although this difference was not statistically significant (p=0.0016), the mean blood loss in the Conventional CS group in our study was larger than the mean blood loss in the Vacuum extraction CS group (382±263.8 mL vs 450±213.97 mL). Like the findings of the study by Arad & Banu et al., there was no significant difference between the two groups Apgar scores.[9]
Like the study by Pelosi et al., the current study shows that complications including an extension of the uterine incision were observed to be much more common in the Vacuum Extraction CS Group[8] In conclusion, using a vacuum extractor connected to the hospital's piped-vacuum supply during a cesarean surgery may be a secure and efficient way to influence the fetal head delivery. This method can make delivery by cesarean section easier.
Conclusion
The results of the study demonstrated that vacuum-assisted Caesarean delivery is superior to manual extraction during Caesarean birth. It was also found that Vacuum Assisted Caesarean Delivery reduced anticipated blood loss, uterine incision extension, and maternal pain. Regarding the Apgar Score, the need for baby resuscitation, or NICU hospitalization, there was no difference between manual and vacuum extraction caesarean births.
Source of Funding
None.
Conflict of Interest
The authors have no conflict of interest to report.
References
- G Molina, TG Weiser, SR Lipsitz, MM Esquivel, T Uribe-Leitz, T Azad. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA 2015. [Google Scholar]
- . . National Family Health Scheme-5 (NFHS-5) . [Google Scholar]
- CY Spong, V Berghella, KD Wenstrom, BM Mercer, GR Saade. Preventing the First Cesarean Delivery: Summary of a Joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol 2012. [Google Scholar]
- E Declercq, R Young, H Cabral, J Ecker. Is a rising cesarean delivery rate inevitable? Trends in industrialized countries. Birth 1987. [Google Scholar]
- RW Mcquivey. Vacuum-assisted delivery: a review. J Matern Fetal Neonatal Med 2004. [Google Scholar]
- UA Ali, ER Norwitz. Vacuum-assisted vaginal delivery. Rev Obstet Gynecol 2009. [Google Scholar]
- R Nakano. Use of the vacuum extractor for delivery of the fetal head at cesarean section. Am J Obstet Gynecol 1981. [Google Scholar]
- MA Pelosi, J Apuzzio. Use of the soft, silicone obstetric vacuum cup for delivery of the fetal head at cesarean section. J Reprod Med 1984. [Google Scholar]
- I Arad, N Linder, B Bercovici. Vacuum extraction at cesarean section--neonatal outcome. J Perinat Med 1986. [Google Scholar]
- C Simonson, P Barlow, N Dehennin, M Sphel, Toppetv, D Murillo. Neonatal complications of vacuum-assisted delivery. Obstet Gynecol 2007. [Google Scholar]
- SL Clark, VL Vines, MA Belfort. Fetal injury associated with routine vacuum use during cesarean delivery. Am J Obstet Gynecol 2008. [Google Scholar]
- C Sakala, YT Yang, MP Corry. Maternity care and liability: pressing problems, substantive solutions. Womens Health Issues 2013. [Google Scholar]
- LB John, S Nischintha, S Ghose. The outcome of forceps delivery in a teaching hospital: A 2-year experience. J Nat Sci Biol Med 2014. [Google Scholar]
- E Solomons. Delivery of the head with the Malmstrom vacuum extractor during cesarean section. Obstet Gynecol 1962. [Google Scholar]
- MJ Lucas. The role of vacuum extraction in modern obstetrics. Clin Obstet Gynecol 1994. [Google Scholar]
- LV Putta, JP Spencer. Assisted vaginal delivery using the vacuum extractor. Am Fam Physician 2000. [Google Scholar]
- R Johanson, V Menon. Soft versus rigid vacuum extractor cups for assisted vaginal delivery. Cochrane Database Syst Rev 2000. [Google Scholar] [Crossref]
- V Apgar. A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg 1953. [Google Scholar]
- S Sritippayawan, W Chantrapitak. Assisted delivery of high floating fetal head: a comparison of vacuum-assisted delivery and manual extraction. Asian Biomed 2011. [Google Scholar]
How to Cite This Article
Vancouver
Agarwal M, Solanki S, Sachau S. Vacuum-assisted caesarean delivery assessment of maternal & fetal outcome [Internet]. Indian J Obstet Gynecol Res. 2023 [cited 2025 Sep 10];10(4):415-420. Available from: https://doi.org/10.18231/j.ijogr.2023.080
APA
Agarwal, M., Solanki, S., Sachau, S. (2023). Vacuum-assisted caesarean delivery assessment of maternal & fetal outcome. Indian J Obstet Gynecol Res, 10(4), 415-420. https://doi.org/10.18231/j.ijogr.2023.080
MLA
Agarwal, Manisha, Solanki, Sweekrati, Sachau, Sumedha. "Vacuum-assisted caesarean delivery assessment of maternal & fetal outcome." Indian J Obstet Gynecol Res, vol. 10, no. 4, 2023, pp. 415-420. https://doi.org/10.18231/j.ijogr.2023.080
Chicago
Agarwal, M., Solanki, S., Sachau, S.. "Vacuum-assisted caesarean delivery assessment of maternal & fetal outcome." Indian J Obstet Gynecol Res 10, no. 4 (2023): 415-420. https://doi.org/10.18231/j.ijogr.2023.080
