- Visibility 94 Views
- Downloads 8 Downloads
- DOI 10.18231/j.ijogr.2023.085
-
CrossMark
- Citation
Role of extended first trimester screening (EFTS) in screening of aneuploidy and prediction of pre-eclampsia
- Author Details:
-
Anima Anjani *
-
Gunjan Rai
-
Gargi Vikas Sharma
-
Shivani Rajouraya
-
Sunil Kumar Chaudhary
Introduction
Enhanced FTS is a new first trimester screening test that employs 4 serum markers, viz. placental growth factor (PlGF), alpha fetoprotein (AFP), pregnancy-associated plasma protein A (PAPP-A), and β-human chorionic gonadotropin (β-hCG) along with the nuchal translucency (NT) measurement and maternal age to generate a pregnancy specific risk for chromosomal abnormalities in the baby, risk of a baby having an open neural tube defect along with the risk of having high blood pressure during the course of pregnancy course (Pre-eclampsia) possibility of having small baby (Fetal Growth Restriction). The quadruple test for fetal aneuploidy (trisomy 21, 18, 13) risk assessment by a combination of maternal age, fetal nuchal translucency thickness (NT) and serum free β-human chorionic gonadotropin (β-hCG) and pregnancy-associated plasma protein A (PAPP-A) can detect about 90% of affected pregnancies at a false-positive rate (FPR) of about 5%.[1] Although, the test is primarily performed for screening of aneuploidy, however, it has got much wider applications as it also helps to identify other pregnancy complications like preeclampsia, gestational diabetes and preterm birth.[2] Among various pregnancy complications preeclampsia has been shown to have a huge impact in terms of pregnancy-related morbidity and mortality that affect nearly one in every twenty pregnant women worldwide.[3] Interestingly, early identification of women at risk of preeclampsia can be managed successfully by administration of low-dose aspirin prior to 16 weeks of pregnancy.[4], [5] Earlier studies have shown upto 90% reduction in early‐onset preeclampsia among women screened and managed using EFTS as compared to those who were not.[6] Keeping in view these promising outcomes, the present study was carried out to evaluate the role of extended first trimester screening (EFTS) in preeclampsia.
Material and Methods
A total of 501 pregnant women aged >18 years attending the antenatal clinic between 11 and 13 weeks of gestation were enrolled in the study after obtaining approval from Institutional Ethics Committee and informed consent from the participants. The minimum sample size projection based on 95% confidence and 80% power was 200, however, we enrolled a total of 501 participants in the study. Women having twin pregnancy and incomplete information about the presence of ART (Assisted reproductive technology), unwilling to undergo screening, those who could come for follow up and delivery were excluded from the study.
At enrolment, clinical history and detailed examination was performed. Maternal blood samples on the same day. Data was prospectively collected on fetal NT and DV-PIV at 11 to 13+6 weeks gestation. Serum specimen were evaluated for b-hCG, Alpha-fetoprotein, PLGF and PAPP-A levels as part of the 11+0 to 13+6 weeks' screening program to determine the risk of preeclampsia and fetal abnormalities. The patients with high risk of developing fetal anomalies were eligible for the process of amniocentesis. However, the patients with low risk of developing fetal anomalies were eligible for phenotypic examination and karyotyping accordingly.
Details of maternal age, sonographic data (CRL and NT) and serum specimen were then transported to commercial facilities offering extended first trimester screening based on the maternal age, sonographic data, and estimation of b-hCG, Alpha-fetoprotein, PLGF and PAPP-A levels. These commercial facilities used specially developed multivariate algorithms to assign the risk of trisomy and preeclampsia. Risk assignment of preeclampsia using PLGF was also done separately by these facilities. Most of these commercial facilities used 1/250 cut-off to assign the risk.
All the women were subsequently followed up for preeclampsia. Assessment of preeclampsia was done after 20 weeks of gestation using the ACOG criteria.[7]
All the pregnancies were managed as per standard ACOG guidelines.[8]
Data so obtained was entered into computer using MS-Excel software and was subjected to statistical analysis.
Data was analyzed using Statistical Package for Social Sciences (SPSS) version 21.0. Chi-square and Independent samples ‘t’-tests were used for analysis of data. ‘p’ value less than 0.05 was considered as significant.
Results
Age of enrolled women ranged from 18 to 49 years. Mean age of women was 28.07±4.77 years. Mean gestational age was 12.21±0.68 weeks. Mean nuchal tube (NT) length was 1.72±0.64 mm. Mean crown-rump length (CRL) was 62±9.52 mm. Nasal bone length was normal in all the cases. Mean right, left and average ductus venosus PI values were 1.01±0.32, 0.91±0.32 and 0.96±0.21 respectively. Median [IQR] b-hCG, AFP, PAPP-A and PLGF were 47.70 [32.11-83.39] ng/ml, 15.01 [11.29-20.45] U/ml, 3755 [2245-5794.5] mIU/L and 57.88 [39.77-79.59] pg/ml respectively. A total of 31 (7.2%) were identified to have intermediate/high risk for T21 trisomy. None of the patients were at T18 or T12 risk according to Quad-test. PLGF was increased in 56 (11.2%) cases. The enhanced first trimester screening (EFTS) was negative in 422 (84.2%) cases. There were 79 (15.8%) cases with EFTS abnormalities. A total of 23 (4.6%) had intermediate/high risk for Down’s syndrome/T21 trisomy, 8 (1.6%) had intermediate/high risk for Down’s syndrome/T21 trisomy along with increased PLGF while 48 (9.6%) had increased PLGF. On prospective follow-up, a total of 14 (2.8%) women developed preeclampsia ([Table 1]).
|
S . No. |
Characteristic |
Statistic |
|
1. |
Mean age±SD (Range) in years |
28.07±4.77 (18-49) |
|
2. |
Mean GA at assesment±SD (Range) weeks |
12.21±0.68 (11-13) |
|
3. |
Sonographic findings |
|
|
Mean NT±SD (Range) in mm |
1.72±0.64 (0.40-3.90) |
|
|
Mean CRL±SD (Range) in mm |
62.00±9.52 (31.60-84.00) |
|
|
Nasal bone length within normal range |
100% |
|
|
Mean DV-PI (Left) |
1.01±0.32 (0.4-1.7) |
|
|
Mean DV-PI (Right) |
0.91±0.32 (0.4-1.8) |
|
|
Mean DV-PI (Average) |
0.96±0.21 (0.60-1.75) |
|
|
4. |
First Trimester Quad-Biochemical tests |
Median [IQR] |
|
b-hCG (ng/ml) |
47.70 [32.11-73.38] |
|
|
AFP (U/ml) |
15.01 [11.29-20.45] |
|
|
PAPP-A (mIU/L) |
3555.00 [2245-5794.5] |
|
|
PLGF (pg/mL) |
57.88 [39.77-79.59] |
|
|
5. |
Risk Assigned for Trisomy and PLGF-risk (No. of cases with intermediate/high risk) |
|
|
T21 risk |
31 (7.2%) |
|
|
T18 risk |
0 |
|
|
T13 risk |
0 |
|
|
PLGF increased risk |
56 (11.2%) |
|
|
6. |
Enhanced First Trimester Screen (EFTS) Status |
|
|
Negative |
422 (84.2%) |
|
|
Positive for Down’s syndrome only/T21 |
23 (4.6%) |
|
|
Positive for PLGF risk only |
48 (9.6%) |
|
|
Positive for both Down’s syndrome/T21 and PLGF risk |
8 (1.6%) |
|
|
7. |
Preeclampsia |
14 (2.8%) |
Evaluating the association of different EFTS components with preeclampsia showed a significant association of preeclampsia with older age (35.75±1.39 years vs 27.85±3.65 years; p<0.001), T21 risk (35.7% vs 5.3%; p<0.001), PLGF risk (57.1% vs 9.9%) and overall quadruple test risk (71.4% vs 14.2%; p = 0.010) respectively. None of the sonographic markers (CRL, DV-PI left, DV-PI right and DV-PI average) showed a significant association with preeclampsia (p>0.05) ([Table 2]).
|
S. No. |
Variable/Parameter |
Preeclampsia (n=14) |
No preeclampsia (n=487) |
Statistical significance |
|
1. |
Mean age±SD (years) |
35.75±1.39 |
27.85±4.65 |
t=6.257; p<0.001 |
|
2. |
Nuchal translucency (mm) |
1.97±0.68 |
1.72±0.63 |
t=1.478; p=0.140 |
|
3. |
CRL (mm) |
59.24±8.02 |
62.07±9.55 |
t=1.018; p=0.309 |
|
4. |
DV-PI (Left) |
0.99±0.36 |
1.01±0.31 |
t=0.232; p=0.816 |
|
5. |
DV-PI (Right) |
1.07±0.23 |
0.91±0.32 |
t=1.744; p=0.082 |
|
6. |
DV-PI (Average) |
1.03±0.08 |
0.96±0.22 |
t=1.122; p=0.262 |
|
7. |
T21 risk (intermediate/ high) |
5 (35.7%) |
26 (5.3%) |
Fisher exact p<0.001 |
|
8. |
PLGF risk |
8 (57.1%) |
48 (9.9%) |
Fisher exact p<0.001 |
|
9. |
Final quadruple test risk |
10 (71.4%) |
69 (14.2%) |
Fisher exact p=0.010 |
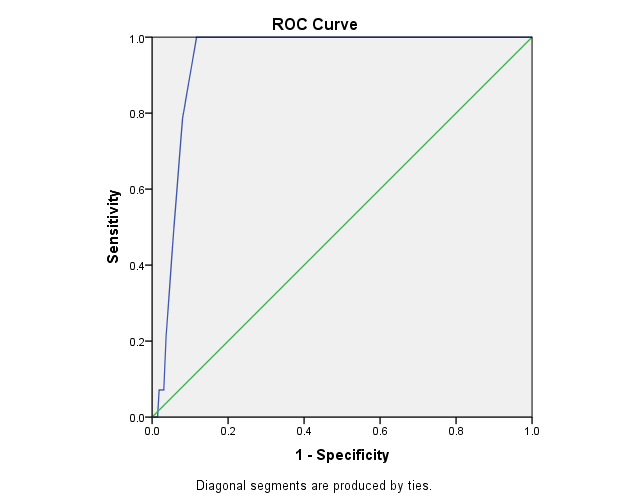
On receiver-operator characteristic (ROC) curve analysis for projection of age as a predictor of preeclampsia, area under the curve value was 0.940±0.012 (p<0.001). The optimum cut-off value at maximum Youden Index (J=0.883) was >33.50 years which was projected to be 100% sensitive and 88.3% specific for prediction of preeclampsia. It had positive and negative predictive values of 19.7% and 100%. The accuracy of age as a predictor of preeclampsia was 88.6%. It had false positivity rate of 11.4% ([Table 3]; [Figure 1]).
|
Area under the cut-off±SE (‘p’ value) |
Youden Index (J) |
Projected Cut-off value |
||
|
0.940±0.012 (p<0.001) |
0.883 |
>33.50 Years |
||
|
Sensitivity |
Specificity |
PPV |
NPV |
Accuracy |
|
100% |
88.3% |
19.7% |
100% |
88.6% |
Among different EFTS components significantly associated with preeclampsia risk, the sensitivity & specificity of age >33.5 years, T21 risk and PLGF risk was 100% & 88.3%, 35.7% & 94.7% and 57.1% & 90.1% respectively with accuracies of 88.6%, 93% and 89.2% respectively. The sensitivity & specificity of presence of any quadruple test risk positivity was 71.4% & 85.8% with an accuracy of 85.4%. The negative predictive value of different independent or combined markers was high and ranged from 98.1% (T21 risk) to 100% (age >33.5 years). Among different EFTS predictors age >33.5 years had maximum positive predictive value (19.7%) whereas combined quadruple test had minimum positive predictive value (12.7%) ([Table 4]).
|
S.No. |
Parameter |
TP |
FP |
FN |
TN |
Sens |
Spec |
PPV |
NPV |
Accuracy |
|
1. |
Age>33.5 years |
14 |
57 |
0 |
430 |
100 |
88.3 |
19.7 |
100 |
88.6 |
|
2. |
T21 risk (intermediate/ high) |
5 |
26 |
9 |
461 |
35.7 |
94.7 |
16.1 |
98.1 |
93.0 |
|
3. |
PLGF risk |
8 |
48 |
6 |
439 |
57.1 |
90.1 |
14.3 |
98.7 |
89.2 |
|
4. |
Any Quadruple test risk |
10 |
69 |
5 |
418 |
71.4 |
85.8 |
12.7 |
99.1 |
85.4 |
Discussion
In the present study, role of extended first trimester screening was assessed in context with preeclampsia. The screened first trimester pregnancies were managed as per standard ACOG guidelines.[8] Consecutively, the incidence of preeclampsia was 2.8% only. As per a recent Government of India report, the incidence of preeclampsia is reported to be 8-10% among the pregnant women. Thus, with the implementation of EFTS guided pregnancy management, we found a substantial reduction in incidence of preeclampsia. First trimester screening for preeclampsia and consequent management of pregnancies helps to reduce the burden of preeclampsia substantially. In an earlier study, Tsiakkas et al. in their study too had a low incidence of preeclampsia for pregnancies assessed at first-trimester. In their study, 3.0% pregnancies developed preeclampsia.[9] However, Sung et al. reported a relatively higher incidence of preeclampsia (6.6%).[10] A better outcome in the present study could be owing to use of extended first trimester screening (EFTS) as compared to use of only single serum markers for risk assessment in these studies.[9], [10]
In the present study, we screened a total of 501 pregnancies, of which T21 aneuploidy risk was assigned to be intermediate in 22 (4.4%) and high in 9 (1.8%) cases. All the pregnancies were marked as low risk for T18 and T12 aneuploidy. Additionally, PLGF increased risk was shown in 56 (11.2%) cases. PLGF is conceived to be associated with increased risk of nonbranching angiogenesis that leads to a low-resistance placental vascular network which in turn could increase the risk of preeclampsia.[11] Thus it could be considered as an independent predictor of preeclampsia.
Compared to the present study, Kwon et al. reported screening test outcomes stratified for three age-groups and collectively instead for separate reporting for trisomy 21 or 18.[12] In their study quad screen test was positive in 6.6%, 16.1% and 36.7% of women aged <35 years, 35-39 years and 40-45 years age groups. Similarly, Yazdani et al. also reported quad screen positive and screen negative results in 34.6% and 65.4% of their patients.[13] Compared to these studies, the results in the present study depicted a relatively lower positivity rate. In the present study, the PLGF increased risk was reported in 11.2% cases. Considering, the independent value of PLGF to be high for prediction of preeclampsia.[14] Thus, we could assume that despite this relatively high projection of preeclampsia risk (as indicated by PLGF risk in >10%) did not transform into actual preeclampsia burden owing to early identification of this risk with help of EFTS and Quadruple tests.
As far as usefulness of these tests for aneuploidy, in the present study, of the nine cases assigned high-risk for Trisomy 21 who comprised only 1.8% of study population. Amniocentesis could be performed in only 6 cases which turned out to be negative in all. Another case in which patient underwent NIPT also resulted in a low risk. Thus, we could not testify the detection rate at all and as such almost all the intermediate or high-risk cases were false-positive. Combined false positivity rate was thus 6.2% (high+intermediate risk) whereas when only high-risk was considered, the false positivity rate was 1.8%.
Despite the false positivity rate of this combined assessment being in agreement with the reported false positive rate of about 5%,[1], [15] we cannot comment over the usefulness of this screening from the point of view of detection of aneuploidy as we did not have any confirmed case of aneuploidy and hence, the sensitivity of the test remained unexplored.
In the present study, none of the cases were detected at risk for trisomies 18 and 13 risk, thus we had a 0% false positive rate for these two.
In the present study, the primary focus of ETFS was on preeclampsia. In the present study, we found that among different independent factors, age had highest sensitivity (100%) while T21 risk had maximum specificity (94.7%). Age criteria had highest accuracy (88.6%). Among different criteria used T21 risk had minimum sensitivity (35.7%) while any EFTS risk had minimum specificity (85.8%). All the predictors had low positive predictive value, ranging from 12.7% (Any EFTS risk) to 19.7% (age >33.5 years), however, negative predictive values were quite high ranging from 98.1% (T21 risk) to 100% (age >33.5 years). As such value of any Extended first-trimester Quadruple-test was 71.4% in terms of sensitivity and 85.8% in terms of specificity for prediction of preelampsia. Its positive and negative predictive values were 12.7% and 99.1%. It was 85.4% accurate.
In fact, these findings highlight the value of age above all the first-trimester quadruple tests either at component level (PLGF risk) or at combined level. Advanced maternal age is a known risk factor for preeclampsia,[16], [17], [18] however, most of these studies described this increased risk at an age of 35 years or above but contrary to that in the present study, age at a cut-off value of only >33.5 years was not only 100% sensitive but was also 88.3% specific. Though, this high sensitivity and specificity of age as a predictor of preeclampsia can be considered to be incidental given the few cases of preeclampsia in event of a low incidence yet this traditional risk factor emerged to be more powerful than the extended first trimester screening (EFTS) or PLGF risk. It may be understood that the value of EFTS and its components in the present study should not be viewed in terms of their predictive efficacy for preeclampsia but instead should be interpreted in terms of their ability to lower down its incidence by adopting appropriate management strategies owing to early assignment of risk. The emergence of older age as the strongest predictor of preeclampsia after adoption of EFTS highlighted some of the limitations where these management strategies need further improvement specific to advanced age pregnancy.
The present study tried to explore the role of first trimester quadruple test for aneuploidy, vis-à-vis extended first trimester screening (EFTS) in preeclampsia and provided some fruitful outcomes that these could help to curb the preeclampsia rate substantially. Further, studies on a larger sample size are recommended.
Conclusion
The findings of the study show that EFTS was helpful in reducing the burden of preeclampsia substantially. Age emerged as a strong predictor of preeclampsia among EFTS screened women thus showing the need for specific management strategies for advanced age pregnancies.
Source of Funding
None.
Conflict of Interest
None.
References
- KH Nicolaides. Screening for fetal aneuploidies at 11 to 13 weeks. Prenat Diagn 2011. [Google Scholar]
- JB Carmichael, HP Liu, D Janik, TW Hallahan, KH Nicolaides, DA Krantz. Expanded conventional first trimester screening. Prenat Diagn 2017. [Google Scholar]
- AB Wallis, AF Saftlas, J Hsia, HK Atrash. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987‐2004. Am J Hypertens 1987. [Google Scholar]
- S Roberge, P Villa, K Nicolaides, Y Giguère, M Vainio, A Bakthi. Early administration of low-dose aspirin for the prevention of preterm and term preeclampsia: a systematic review and meta-analysis. Fetal Diagn Ther 2012. [Google Scholar]
- S Roberge, K Nicolaides, S Demers, J Hyett, N Chaillet, E Bujold. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis. Am J Obstet Gynecol 2017. [Google Scholar]
- F Park, K Russo, P Williams, M Pelosi, R Puddephatt, M Walter. Prediction and prevention of early-onset pre-eclampsia: impact of aspirin after first-trimester screening. Ultrasound Obstet Gynecol 2015. [Google Scholar]
- . Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol 2020. [Google Scholar]
- . ACOG Committee Opinion No. 743: Low-Dose Aspirin Use During Pregnancy. Obstet Gynecol 2018. [Google Scholar]
- A Tsiakkas, R Cazacu, A Wright, D Wright, KH Nicolaides. Maternal serum placental growth factor at 12, 22, 32 and 36 weeks' gestation in screening for pre-eclampsia. Ultrasound Obstet Gynecol 2016. [Google Scholar]
- KU Sung, JA Roh, KJ Eoh, EH Kim. Maternal serum placental growth factor and pregnancy-associated plasma protein A measured in the first trimester as parameters of subsequent pre-eclampsia and small-for-gestational-age infants: A prospective observational study. Obstet Gynecol Sci 2017. [Google Scholar]
- S Agrawal, S Shinar, AS Cerdeira, C Redman, M Vatish. Predictive Performance of PlGF (Placental Growth Factor) for Screening Preeclampsia in Asymptomatic Women: A Systematic Review and Meta-Analysis. Hypertension 1979. [Google Scholar]
- JY Kwon, IY Park, SM Kwon, CJ Kim, JC Shin. The quadruple test for Down syndrome screening in pregnant women of advanced maternal age. Arch Gynecol Obstet 2012. [Google Scholar]
- S Yazdani, R Rouholahnejad, N Asnafi, M Sharbatdaran, M Zakershob, Z Bouzari. Correlation of pregnancy outcome with quadruple screening test at second trimester. Med J Islam Repub Iran 2015. [Google Scholar]
- S Agrawal, S Shinar, AS Cerdeira, C Redman, M Vatish. Predictive Performance of PlGF (Placental Growth Factor) for Screening Preeclampsia in Asymptomatic Women: A Systematic Review and Meta-Analysis. Hypertension 1979. [Google Scholar]
- D Wright, KO Kagan, FS Molina, A Gazzoni, KH Nicolaides. A mixture model of nuchal translucency thickness in screening for chromosomal defects. Ultrasound Obstet Gynecol 2008. [Google Scholar]
- GA Tessema, A Tekeste, TA Ayele. Preeclampsia and Associated Factors Among Pregnant Women Attending Antenatal Care in Dessie Referral Hospital, Northeast Ethiopia: A Hospital-Based Study. BMC Pregnancy Childbirth 2015. [Google Scholar]
- D Shan, PY Qiu, YX Wu, Q Chen, AL Li, S Ramadoss. Pregnancy Outcomes in Women of Advanced Maternal Age: a Retrospective Cohort Study from China. Sci Rep 2018. [Google Scholar] [Crossref]
- K Ogawa, KY Urayama, S Tanigaki, H Sago, S Sato, S Saito. Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC Pregnancy Childbirth 2017. [Google Scholar]
