- Visibility 31 Views
- Downloads 5 Downloads
- DOI 10.18231/j.ijogr.2024.011
-
CrossMark
- Citation
Efficacy of 2D/3D HyCoSy with new contrast medium lignocaine and saline comparing with HSG - A single centre prospective study
- Author Details:
-
Chegondi V Narayana Rao *
-
Sindhu Chegondi
-
Murali Krishna Kota
Introduction
The fallopian tubes serve as crucial conduits for the transportation of gametes and embryos. Tubal issues contribute to 25%-35% of cases involving couples with subfertility.[1] In India, prevalent conditions such as pelvic inflammatory disease, chronic infections, and genital tract tuberculosis are known to impact women's infertility rates.[2] While laparoscopic examination with chromo-pertubation dye test (LDT) is considered the gold standard for tubal assessment, it entails invasiveness and drawbacks including anesthesia-associated risks, patient hospitalization due to methylene blue usage, surgical complications, and high costs. Traditional utilization of hysterosalpingography (HSG) has been employed to assess both the uterine cavity and tubal condition.[3] It necessitates the use of iodinated contrast medium, which can trigger allergic reactions and presents concerns related to radiation exposure. Furthermore, it is unable to assess conditions such as ovarian or uterine pathologies like leiomyomas or adenomyosis. Both HSG and LDT exhibit numerous drawbacks and significant limitations, underscoring the potential for an alternative technique to address these issues.
Initially, hysterosalpingo-contrast sonography (HyCoSy) faced limited clinical adoption due to inadequate visualization and concerns regarding radiation exposure in its early developmental stages.[4] However, Nanani et al[4] pioneered the utilization of HyCoSy for assessing tubal patency back in 1981, and it has since become widely favored as a primary imaging technique. Both Nannini et al[4] and Volpi et al[3] noted that the saline solution introduced into the endometrial cavity illuminated intrauterine structures by virtue of the surrounding fluid detected through transvaginal ultrasound. Throughout this procedure, they observed fluid in the pouch of Douglas (POD), indicating the flow of fluid through the patent fallopian tubes, a method recognized as saline infusion sonography (SIS). Nevertheless, this method does not provide insights into the precise location of the blockage, the condition of the tubal lumen, or the tubo-ovarian relationship. To address these limitations, a combination of air and saline has been employed as an ultrasound contrast medium.[5] Moreover, advancements have been made in ultrasound contrast agents, evolving from negative contrast agents like normal saline to positive contrast agents such as microbubble agents like echovist and sonoview. [5] Another variant involves the utilization of a foam created by mixing Ex-Em gel with saline (ExEm gel® by Gynecologiq BV, Delft, The Netherlands), which contains hydroxyethyl cellulose and glycerol, referred to as HyFoSy.[6] HyCoSy and HyFoSy offer distinct advantages compared to other methods, as they incorporate the principles of both SIS and HSG. The challenges associated with using a saline medium have been effectively addressed through the application of contrast or foam, enabling comprehensive assessment of the entire tubal pathway and detecting partial obstructions indicative of tubal damage. However, the visualization of both right and left tubes in a single plane remains difficult in numerous cases due to the tubes' variable positioning.[7], [8], [9] Echogenic bowels surrounding the tubes and spill can obscure the visualization. Additionally, the initial dispersion of the contrast agent within the pelvic cavity frequently disrupts the contrast image, presenting limitations inherent to 2D HyCoSy. These constraints can be surmounted through the adoption of 3D HyCoSy. HyCoSy presents as a user-friendly and safe technique, obviating the need for hospitalization. However, the cost and availability of ultrasound contrast agents have hindered its widespread use until recent times.[10]
The constraints linked to various techniques and procedural challenges prompted the initiation of this current study, with the aim of formulating a novel contrast medium that is not only cost-effective but also accessible to all categories of infertile women, regardless of their financial circumstances. The study is designed to assess and compare the diagnostic precision of 2D/3D HyCoSy employing lignocaine as a contrast gel with the established conventional method of HSG (using dye as the contrast medium) for evaluating tubal patency.
Materials and Methods
Study design
A prospective, observational, non-randomized study on 117 infertile women who came to Shilpa Scan Centre in Palakollu, Andhra Pradesh, India from May 2017 to May 2022 to test their tubal patency was conducted to investigate infertility.
Inclusion and exclusion criteria
Inclusion criteria encompassed women aged 19-45 years partnered with males exhibiting normal semen analysis results. Exclusion criteria comprised present vaginal infections, a history of uterine bleeding, prior surgical cases, significant multiple fibroids, husbands with Azoospermia or oligospermia, and lack of consent for participation.
Instruments
The process was executed utilizing Wipro GE Voluson E10 and E8 systems, both equipped with endovaginal probes of 5-9 MHz and 6-12 MHz 3D capabilities (GE Healthcare, USA).
Contrast preparation
In our investigation, we employed a contrast consisting of a mixture of lignocaine gel and saline. This 2% lignocaine gel, which holds FDA approval, is a sterile aqueous solution containing preservatives such as methylparaben and propylparaben, along with hypromellose. It is available as a sterile preparation. Lignocaine gel finds application in catheterization, endoscopies, gynecologic examinations, as well as rectal and colon examinations. Extensive testing has confirmed the safety of this gel and its constituents in medical use.
The gel preparation procedure proceeded as follows: 25ml of saline was drawn into a 50cc catheter tip syringe, and 4ml of 2% lignocaine gel was drawn into a 10cc syringe. These two syringes were then connected, and the gel was vigorously pushed through the small openings in the syringes. This vigorous movement created turbulence, leading to a decrease in local pressure which, in turn, caused air to dissolve in the solution, forming small air bubbles. These air bubbles, visible on ultrasound as echogenic specks, coalesced to create a stable, whitish foam contrast medium, which maintained its integrity for several minutes.
The viscosity of the contrast medium was appropriately low, facilitating easy passage through the narrow lumen of fallopian tubes, while the suspended air bubbles remained visible for a duration of at least 5-7 minutes. Just before administration, the final concentration was adjusted to 0.2% lignocaine by dilution with normal saline. Once within the abdominal cavity, this foam was gradually absorbed into the tubes after the procedure was completed.
The contrast medium utilized in the study has been granted a patent for an invention titled "Contrast Medium and Methods for Its Preparation for Assessing Conduit Patency." This patent, bearing the number 419915, is valid for a period of 20 years from 8th July 2016, in accordance with the provisions outlined in the Patent Act of 1970 (Supplement Material).
Study preparation
Both the HyCoSy and HSG procedures were conducted during the follicular phase (6-11 days of the menstrual cycle) and only after confirming a negative pregnancy test. To manage potential discomfort during the procedure, participants were administered a test dose of lignocaine followed by a 2 ml intramuscular injection of diclofenac. Prior to the procedure, a baseline ultrasound study was performed to comprehensively assess the uterus and adnexa. The procedure itself was executed with the patient in a lithotomy position, maintaining stringent aseptic precautions. A speculum was inserted into the patient's vagina, and an 8F pediatric Foley's catheter was introduced into the endometrial cavity, with the bulb being inflated using 0.5 ml of water. Subsequently, an ultrasound transducer was introduced into the vaginal canal to visualize the uterus in the longitudinal plane. Both the HyCoSy and HSG procedures were performed in the same sitting for the patients.
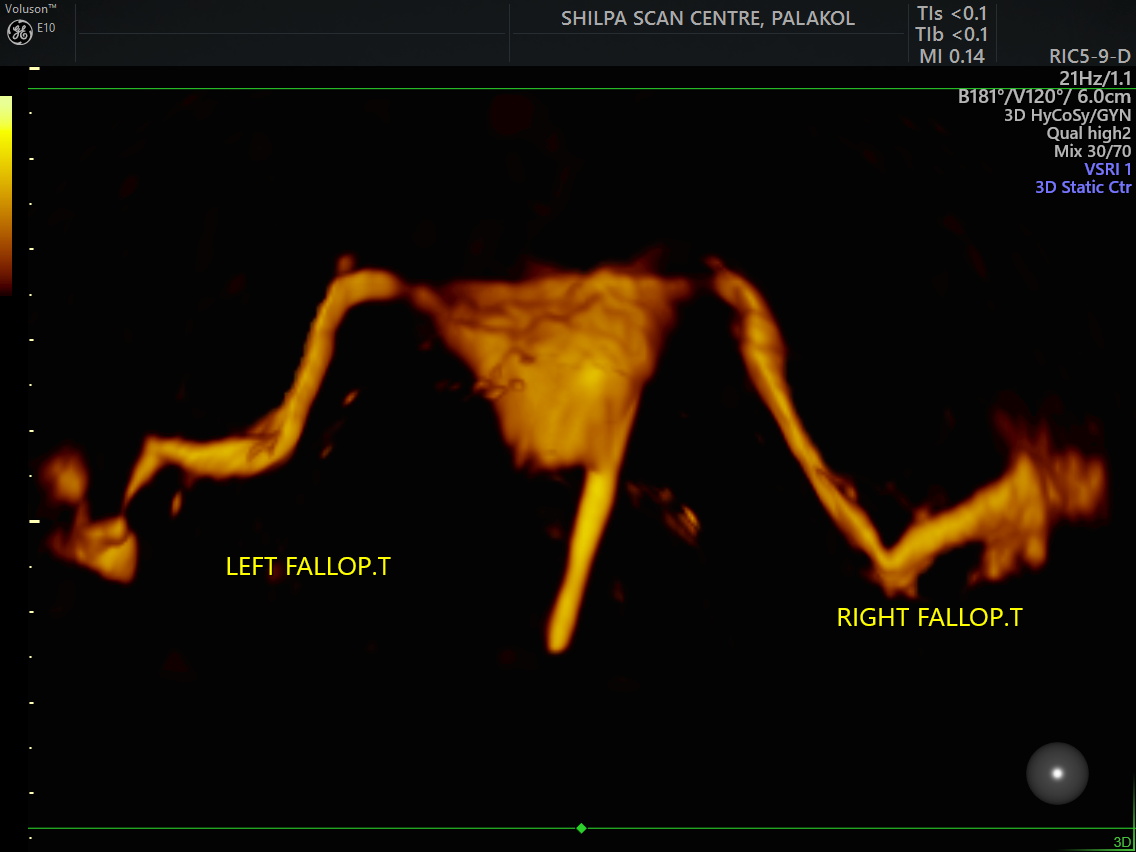
Subsequently, the foam was introduced into the uterine cavity by gently pressing the syringe's plunger, assisted by a light touch. Upon confirming the presence of foam within the uterine cavity along the longitudinal axis, the transducer was rotated to a transverse orientation to capture a visual of the Fallopian tubes' distension on both sides ([Figure 1]). The dispersion pattern of the foam within the peritoneal cavity was more easily discernible after pinpointing the location of the ovaries. Throughout the examination, continuous assessment was carried out to monitor participants' safety, documenting any adverse effects and instances of discomfort. Concluding the procedure, the balloon was deflated and the catheter was removed. For the 2D scan, an angle of 180º was set, while the 3D volume scan utilized an angle of 120º.
Key indicators to identify tubal patency within the framework of 3D HyCoSy encompass:
Turbulent flow sign: Continuous forward flow observed in the proximal section of the tubes, maintaining for a minimum of 15 seconds.
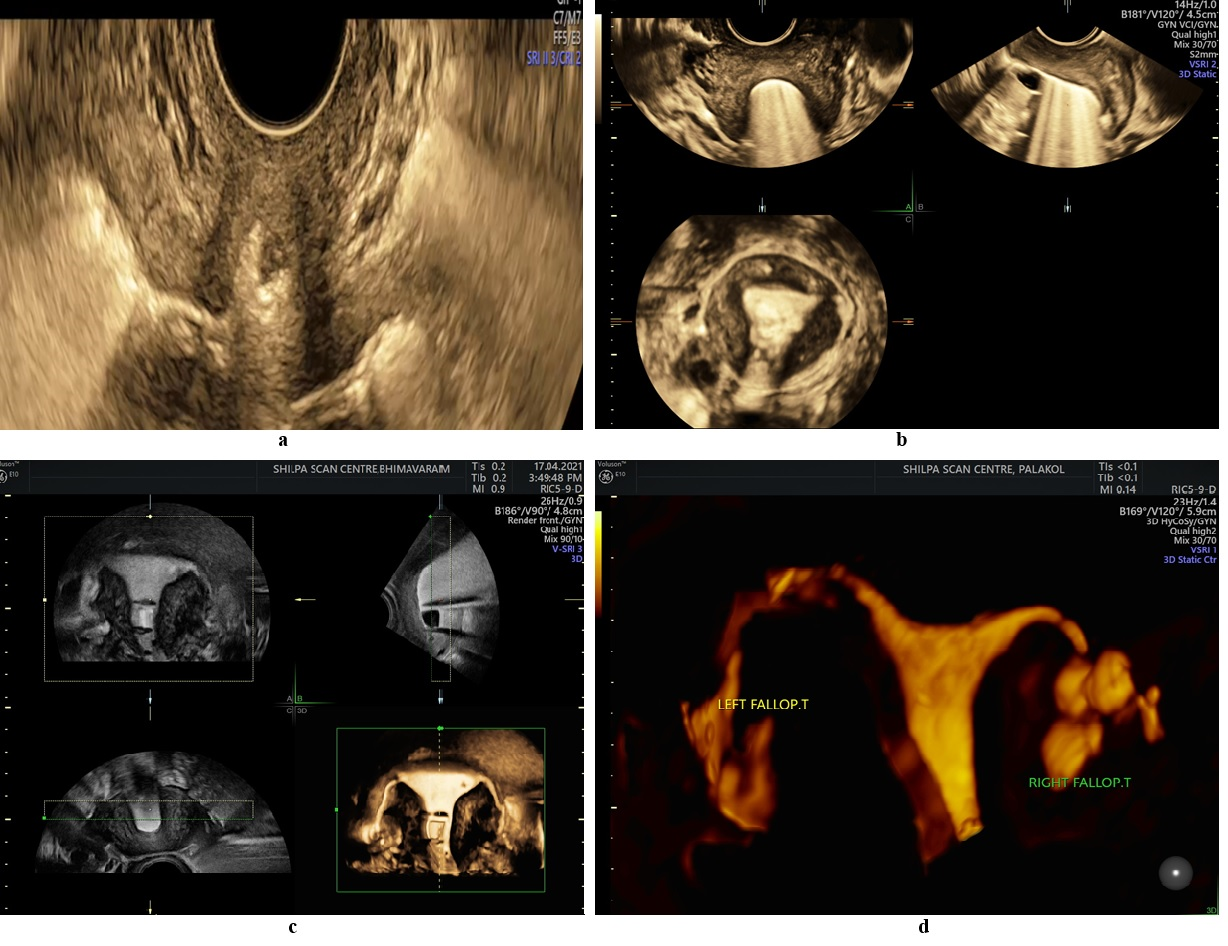
Shower sign: Contrast observed along the entire length of the tube, with foam dispersing into the peritoneal cavity through the fimbrial ends in a shower-like pattern ([Figure 2] a).
Ring sign: Presence of air bubbles enveloping the ovary, accompanied by contrast within the pouch of Douglas ([Figure 2] b). Employing the 2D/3D HyCoSy modality facilitated capturing a comprehensive view of the pelvic cavity in a single sweep. This allowed for the observation of morphological traits of the uterine cavity, tube shapes, tubal surface, and coiling of the tubes ([Figure 2] c). Additionally, advanced indications such as Tuberculus Salpingitis, Hydrosalpinx ([Figure 2] d), and the Nodosa-beaded appearance were identifiable, alongside any uterine anomalies. In instances of tube occlusion, an increased resistance is encountered during contrast injection due to the contrast's backflow, coupled with the non-visualization of echogenic tubes. Notably, obstructed tubes manifest strong echogenic star-like patterns penetrating the myometrium (intravasation).
Assessment of false positive and false negative
False positive (false patency) results can occur in the following scenarios. Firstly, bilateral cornual blockage can induce increased pressure of contrast within the uterine cavity, causing intravasation into extrauterine vessels, which may mimic tubal patency. Secondly, contrast may follow a pathway along the pouch of Douglas from a patent tube to the contralateral side, creating the impression of bilateral tubal patency. Employing meticulous techniques can mitigate these issues. It is crucial to observe the contrast flow pattern in relation to its injection site. Additionally, tracking the contrast flow from the cornual region distally and ensuring its antegrade direction are both important.
Conversely, false occlusion (false negative) results can be attributed to various factors. Firstly, tubes may experience temporary occlusion due to factors like a mucous plug, myometrial spasm, blood clot, or mucosal edema. The proximal tube, particularly susceptible to this, can exhibit temporary cornual blockage. Secondly, technical challenges, such as contrast leakage or cervical stenosis, may lead to an inability to achieve the necessary pressure for hydrotubation. Tubal convolution or altered anatomy resulting from pelvic adhesions can also complicate the tracking of the fallopian tubes.
Pain disturbances
Participants in the study were instructed to communicate any discomfort or pain they encountered during the diagnostic procedure. They were asked to provide feedback immediately after the procedure and again 24 hours later. Pain intensity and severity were evaluated using a 'Numerical Rating Scale (NRS)' ranging from 0 to 10. The NRS comprises ten questions in the questionnaire, with pain levels assessed and scored between 0 and 10. These scores were then categorized as mild, moderate, or severe, as outlined in [Table 1].
|
Verbal Score |
Grade |
|
0 |
None |
|
1-3 |
Mild |
|
4-6 |
Moderate |
|
7-10 |
Severe |
Statistical interpretation
Data organization was carried out using Microsoft Excel, while statistical analysis was conducted using IBM SPSS Statistics for Windows, Version 25.0 (Armonk, NY: IBM Corp.) software. The key parameters assessed were specificity, sensitivity, positive predictive value, and negative predictive value. Descriptive variables such as Mean, Standard Deviation, and Percentages were calculated, with significance levels denoted by P values less than 0.05. The Chi-Square test was employed to identify any trends indicated by the P values.
Ethical approval
The study protocol obtained approval from the Institutional Ethics Committee of Holistic Health Care & Research Centre under Register Number ECR/284/Indt/AP/2017. Participants were provided with a comprehensive explanation of the tubal patency procedure, and their consent, along with that of their guardians, was secured through the utilization of Informed Consent Forms. All data was collected, documented, and secured in adherence to established protocol.
Results
Demographic and clinical characteristics of participants
A total of 117 women with a history of infertility were encompassed in this study. The average age of the participants was 27.79 ± 4.29 years, ranging from 19 to 45 years, and their mean duration of active marital life was 8.46 ± 4.42 years. In terms of overall occurrence, secondary infertility was more predominant (n = 64, 54.7%) than primary infertility (n = 53, 45.2%) ([Table 3]). Analyzing the distribution across age groups revealed that both primary and secondary infertility were more frequent within the 26-30 age bracket ([Table 2]).
|
Age group (years) |
Primary N (%) |
Secondary N (%) |
Total |
Chi-square test P-value |
|
19-25 |
23 (19.6) |
17 (14.5) |
40 |
0.465 |
|
26-30 |
23 (19.6) |
28 (23.9) |
51 |
|
|
31-35 |
5 (4.2) |
18 (15.3) |
23 |
|
|
36-45 |
2 (1.7) |
1 (0.8) |
3 |
|
|
Total |
53 |
64 |
117 |
Within the participant pool, the largest group of women (31.6%) had a background of irregular menstrual cycles. Among them, 22 patients (18.8%) were diagnosed with PCODs, while 12 patients (10.2%) exhibited single to multiple uterine fibroids. Additional conditions identified included ovarian cysts (11.1%), chocolate cysts (6.8%), and cervical stenosis (4.2%) ([Table 3]). Furthermore, four patients underwent post-tubectomy recanalization, and seven patients were found to have endometrial polyps.
|
Demographic factors |
Mean ± SD |
|
|
Age (years) |
27.79 ± 4.29 |
|
|
AML (years) |
8.46 ± 4.42 |
|
|
Primary infertility, n (%) |
53 (45.2%) |
|
|
Secondary infertility, n (%) |
64 (54.7%) |
|
|
Female infertility parameter n % |
||
|
Irregular menstruation |
37 |
31.62 |
|
PCOD |
22 |
18.80 |
|
Ovarian cysts |
13 |
11.11 |
|
Uterine fibroids |
12 |
10.25 |
|
Chocolate cysts |
8 |
06.83 |
|
Cervical stenosis |
5 |
04.27 |
|
Endometrial polyps |
7 |
05.98 |
Tubal patency evaluation
The diagnostic accuracy outcomes for tubal occlusion revealed that the 2D/3D HyCoSy procedure employing 2% lignocaine gel exhibited a sensitivity of 91.86%, specificity of 89.18%, positive predictive value of 90.40%, and negative predictive value of 90.82%, when compared to the conventional HSG method ([Table 4]). In terms of right tubal patency, HyCoSy displayed a sensitivity of 92.30% and specificity of 88.46%. Additionally, HyCoSy yielded results indicating false-negative findings in 5 cases and false-positive findings in 6 cases ([Table 5]), with an overall accuracy of 90.59%.
|
Accuracy finding parameters |
Percentage (%) |
|
Specificity |
89.18% |
|
Sensitivity |
91.86% |
|
Predictive value of positive test |
90.40% |
|
Predictive value of negative test |
90.82% |
|
Percentage of false positives |
10.81% |
|
Percentage of false negatives |
08.13% |
|
HyCoSy Vs HSG (Right tube) |
|||||
|
|
HSG |
Total |
P-value |
||
|
Positive |
Negative |
||||
|
HyCoSy |
Positive |
60 |
6 |
66 |
0.001* |
|
Negative |
5 |
46 |
51 |
||
|
Total |
65 |
52 |
117 |
The examination of left tubal patency using HyCoSy indicated 6 false-positive cases and 5 false-negative cases, resulting in a sensitivity of 91.37%, specificity of 89.83%, and accuracy of 90.59% ([Table 6]). The comprehensive evaluation of tubal patency for both tubes combined is presented in [Table 7]. Notably, the diagnostic performance of 2D/3D HyCoSy demonstrated notably high sensitivity (91.86%), specificity (89.18%), and accuracy (90.59%). However, the analysis also unveiled 12 instances of false-positive results and 10 instances of false-negative results for HyCoSy. [Table 8] illustrates the assessment of HyCoSy's diagnostic accuracy in the overall determination of tubal patency (including right, left, and combined) when compared to the conventional HSG as the gold standard. The collective outcome indicated an overall diagnostic accuracy of 90.59%.
|
HyCoSy Vs HSG (Left tube) |
|||||
|
|
HSG |
Total |
P-value |
||
|
Positive |
Negative |
||||
|
HyCoSy |
Positive |
53 |
6 |
59 |
0.001* |
|
Negative |
5 |
53 |
58 |
||
|
Total |
58 |
59 |
117 |
|
HyCoSy Vs HSG (Combined) |
|||||
|
|
HSG |
Total |
P- value |
||
|
Positive |
Negative |
||||
|
HyCoSy |
Positive |
113 |
12 |
125 |
0.003 |
|
Negative |
10 |
99 |
109 |
||
|
Total |
123 |
111 |
234 |
|
Study procedure |
Hysterosalpingography (HSG) |
|
||||||
|
|
True positive |
False positive |
True negative |
False negative |
Sensitivity % |
Specificity % |
Accuracy % |
|
|
HyCoSy |
Right tube finding |
60 |
6 |
46 |
5 |
92.30 |
88.46 |
90.59 |
|
Left tube finding |
53 |
6 |
53 |
5 |
91.37 |
89.83 |
90.59 |
|
|
Both tube finding |
113 |
12 |
99 |
10 |
91.86 |
89.18 |
90.59 |
Statistical analysis involved utilizing the Chi-Square test at P trend, with significance considered for values below 0.05. Significance was observed in the P trend for the right, left, and combined fallopian tube assessments, with levels of 0.001, 0.001, and 0.003 respectively ([Table 5], [Table 6], [Table 7]).
Pain score
The utilization of the 2D/3D HyCoSy technique with 2% lignosal gel yielded lower pain intensity, as assessed through a scoring and grading methodology. Pain disturbances categorized as "None - Mild" during 2D/3D HyCoSy accounted for 83.48%, while for HSG, the corresponding figure was 45.63%. On the other hand, the prevalence of moderate to severe pain discomforts was 16.33% during 2D/3D HyCoSy and 91.26% during HSG. The experienced discomforts during the study may be attributed to uterine distension following the infusion of the saline solution, leading to the release of prostaglandins and subsequent uterine cramping. Administering a diclofenac injection prior to commencing the procedure, combined with the localized anesthetic effect of the lignosal contrast, contributed to alleviating pain disturbances during the diagnostic procedure.
Discussion
The prevalence of female infertility has seen a significant rise in recent years. Ensuring precise and reliable assessment of tubal patency holds paramount importance for diagnosing and addressing infertility. HSG and HyCoSy are two widely employed, dependable, and non-invasive imaging methods for evaluating tubal patency. The integration of contrast and 2D/3D technology has further enhanced the accuracy of HyCoSy. However, HSG remains a preferred option for many due to its notable specificity. Taking these factors into consideration, we formulated a diagnostic accuracy study to juxtapose HyCoSy with lignocaine gel as a contrast against the conventional HSG test. The study participants fell within the age range of 19 to 45 years, with a mean age of 27.79. Notably, secondary infertility exhibited a higher prevalence rate (54.7%) in comparison to primary infertility (45.2%).
The diagnostic accuracy assessment of 2D/3D HyCoSy utilizing 2% lignosal gel yielded a sensitivity of 91.86%, specificity of 89.18%, a positive predictive value of 90.40%, and a negative predictive value of 90.82%. Based on a review article stemming from a workshop held in Las Vegas in 1993, which aimed to evaluate HyCoSy's efficacy using positive echocontrast agents for reliable tubal patency assessment and its potential role in infertility investigations, [11] the study reported a detection rate of 100% for occluded tubes and 86% for patent tubes. The current study's outcomes were in alignment with prior research. For instance, the work by Marcos M. Reis et al [12] conducted a comparison between HyCoSy with echovist and HSG, yielding a concordance value of 76.1%. Another study indicated that using HyFoSy for tubal patency assessment could potentially eliminate the need for HSG in around 78% of infertility cases. [6] Moreover, a systematic review of past studies demonstrated a high diagnostic accuracy of 3D HyCoSy, boasting a sensitivity of 98% and specificity of 90%.[13] However, these results deviated from earlier studies where the sensitivity, specificity, and diagnostic predictive values of HyCoSy and HSG were comparable in diagnosing tubal block.[13], [14], [15]
Numerous investigations have consistently indicated superior outcomes for tubal obstruction assessment with both 2D HyCoSy and 3D HyCoSy. [6], [10], [13] In alignment with these findings, our study also revealed notable diagnostic efficacy of 2D/3D HyCoSy in comparison to HSG for diagnosing tubal patency in both tubes. This was underscored by the elevated sensitivity, specificity, and accuracy values of 91.86%, 89.18%, and 90.59%, respectively. The integration of 3D imaging permits comprehensive visualization of fallopian tubes, mitigating the occurrence of false patency outcomes that can arise with 2D HyCoSy in complexly convoluted tubes.[16] The investigation unveiled that the utilization of 2D/3D HyCoSy with lignosal presented a well-tolerated diagnostic procedure, resulting in minimal pain intensity for participants in comparison to menstrual cramp discomfort. Notably, the employment of the gel caused less discomfort than the saline solution, delivering slightly improved uterine cavity distension and enhanced image clarity.
While some authors might propose that HyCoSy is not entirely accurate as a replacement for HSG, our study established that HyCoSy with lignosal stands as a viable substitute. [3] This method proves to be more convenient, safer, and carried out in a single outpatient setting, effectively minimizing fertility assessment expenses. It offers the ability to evaluate uterine anomalies linked to infertility and pinpoint the precise location for identifying tubal obstructions. This innovative procedure presents numerous advantages over HSG in the realm of diagnosing tubal patency.
Conclusion
Based on the findings of the present study, it can be concluded that 2D/3D HyCoSy with lignocaine gel demonstrates notable sensitivity and specificity in detecting tubal patency among infertility patients. A significant advantage of HyCoSy is its avoidance of radiation and iodine exposure, distinguishing it favorably from HSG. Moreover, the 2D/3D HyCoSy technique with lignosal proves to be cost-effective in comparison to HyCoSy using microbubble contrast agents like echovist and sonoview. Consequently, the utilization of HyCoSy with lignocaine gel as a contrast technique emerges as a promising alternative diagnostic tool in infertility treatment, exhibiting enhanced accuracy and effectiveness when juxtaposed with conventional HSG.
Patent Grants
The contrast medium used in the study, got patent grants for an invention entitled “Contrast Medium and methods involved in preparation for the determination of patency of Conduits” with patent number 419915, for the term of 20 years from 8th July 2016 in accordance with the provisions of the Patent Act, 1970 (Supplement Material).
Study Limitations
A limitation of this study is the relatively small sample size, which poses challenges in achieving a precise evaluation. Consequently, further randomized studies are warranted to validate and enhance the accuracy and effectiveness of the 2D/3D HyCoSy technique with lignocaine gel.
Source of Funding
This study was self-funded, with no external sources of financial support.
Conflict of Interest
The present study did not involve any conflicts of interest.
References
- PJ Rowe, FH Comhaire, TB Hargreave, AM Mahmoud. . WHO manual for the standardized investigation and diagnosis of the infertile male 2000. [Google Scholar]
- C Gnoth, E Godehardt, P Frank-Herrmann, K Friol, J Tigges, G Freundl. Definition and prevalence of subfertility and infertility. Hum Reprod 2005. [Google Scholar]
- OA Omidiji, OO Toyobo, O Adegbola, A Fatade, OA Olowoyeye. Hysterosalpingographic findings in infertility-what has changed over the years?. Afr Health Sci 2019. [Google Scholar]
- R Nannini, E Chelo, F Branconi, C Tantini, G F Scarselli. Dynamic echohysteroscopy: a new diagnostic technique in the study of female infertility. Acta Eur Fertil 1981. [Google Scholar]
- P Jeanty, S Besnard, A Arnold, C Turner, P Crum. Air-contrast sonohysterography as a first step assessment of tubal patency. J Ultrasound Med 2000. [Google Scholar]
- MH Emanuel, MV Vliet, M Weber, N Exalto. First experiences with hysterosalpingo-foam sonography (HyFoSy) for office tubal patency testing. Hum Reprod 2012. [Google Scholar]
- DV Schoubroeck, TV Bosch, C Meuleman, C Tomassetti, T D'Hooghe, D Timmerman. The use of a new gel foam for the evaluation of tubal patency. Gynecol Obstet Invest 2013. [Google Scholar]
- C Exacoustos, AD Giovanni, B Szabolcs, H Binder-Reisinger, C Gabardi, D Arduini. Automated sonographic tubal patency evaluation with three-dimensional coded contrast imaging (CCI) during hysterosalpingo-contrast sonography (HyCoSy). Ultrasound Obstet Gynecol 2009. [Google Scholar]
- C Exacoustos, AD Giovanni, B Szabolcs, V Romeo, ME Romanini, D Luciano. Automated three-dimensional coded contrast imaging hysterosalpingo-contrast sonography: feasibility in office tubal patency testing. Ultrasound Obstet Gynecol 2013. [Google Scholar]
- D Aggarwal. Can HyCoSy replace laparoscopy and hysteroscopy as a method to assess tubal patency and uterine cavity lesions. IOSR J Dent Med Sci 2019. [Google Scholar]
- S Campbell, TH Bourne, SL Tan, WP Collins. Hysterosalpingo contrast sonography (HyCoSy) and its future role within the investigation of infertility in Europe. Ultrasound Obstet Gynecol 1994. [Google Scholar]
- MM Reis, SR Soares, ML Cancado, AF Camargos. Hysterosalpingo contrast sonography (HyCoSy) with SH U 454 (Echovist) for the assessment of tubal patency. Hum Reprod 1998. [Google Scholar]
- JL Alcázar, TM Corral, R Orozco, J Dominguez-Piriz, L Juez, T Errasti. Three-Dimensional Hysterosalpingo-Contrast-Sonography for the Assessment of Tubal Patency in Women with Infertility: A Systematic Review with Meta-Analysis. Gynecol Obstet Invest 2016. [Google Scholar]
- M Dietrich, A Suren, B Hinney, R Osmers, W Kuhn. Evaluation of tubal patency by hysterocontrast sonography (HyCoSy, Echovist®) and its correlation with laparoscopic findings. J Clin Ultrasound 1996. [Google Scholar]
- HO Hamed, AY Shahin, AM Elsamman. Hysterosalpingo-contrast sonography versus radiographic hysterosalpingography in the evaluation of tubal patency. Int J Gynaecol Obstet 2009. [Google Scholar]
- CV Rao, C Sindhu, MK Kota. Three-dimensional Hysterosalpingo Contrast Sonography with Lignosal as Contrast for Evaluation of Tubal Patency in the Infertile Women-An Observational Cohort Study. Am J Sonography 2019. [Google Scholar]
- Introduction
- Materials and Methods
- Study design
- Inclusion and exclusion criteria
- Instruments
- Contrast preparation
- Study preparation
- Assessment of false positive and false negative
- Pain disturbances
- Statistical interpretation
- Ethical approval
- Results
- Discussion
- Conclusion
- Patent Grants
- Study Limitations
- Source of Funding
- Conflict of Interest
