- Visibility 77 Views
- Downloads 9 Downloads
- DOI 10.18231/j.ijogr.2025.027
-
CrossMark
- Citation
Introduction
Vulvar tumours are uncommon tumour of the lower genital tract and a frequent cause for gynaecologic consultation. Most require no treatment or might require simple excision. Common differential diagnoses to be considered are infectious cause, pre-malignant and malignant tumours and skin cancers.[1]
Vulvar tumours mostly have benign features and require complete clinical, pathological examination to exclude premalignant or malignant lesions.[2]
Clinically vulvar tumours can be classified as cystic and solid tumours. Cystic like Bartholin’s cyst or abscess, canal of Nuck cyst, Skene cyst, vestibular mucous cyst and solid tumours like lipoma, angiomas, vulvar carcinoma.[1]
The recognition of vulvar lesions and differentiation between benign, pre-malignant and malignant stages are important for diagnosis, monitoring and treatment.[3]
In this case series of rare benign vulvar tumours – 3 cases are discussed – vulvar angiofibroma, phyllodes tumour of the vulva and haemangioma of the vulva.
Angiofibroma of Vulva
Angiofibroma is a site specific, benign mesenchymal neoplasm with a genitourinary region predilection. It is a rare vulvar tumour usually noted in middle aged women.[4]
It is characterised by 2 components – a spindle cell component and medium sized vessels with mural hyalinization. This condition has good prognosis and can be cured by local excision.[5]
Case report 1
Here is a rare case report of a young patient with vulvar mass.
A 20-year-old presented with complaints of mass in genital region in the last 6 months. ([Figure 1] A) Initially the size of a pea, gradually progressed to 4x5cm. Patient had no complaints of pain, itching, no discharge from the swelling. Patient had no history of fever, burning micturition, and no significant past or family history.
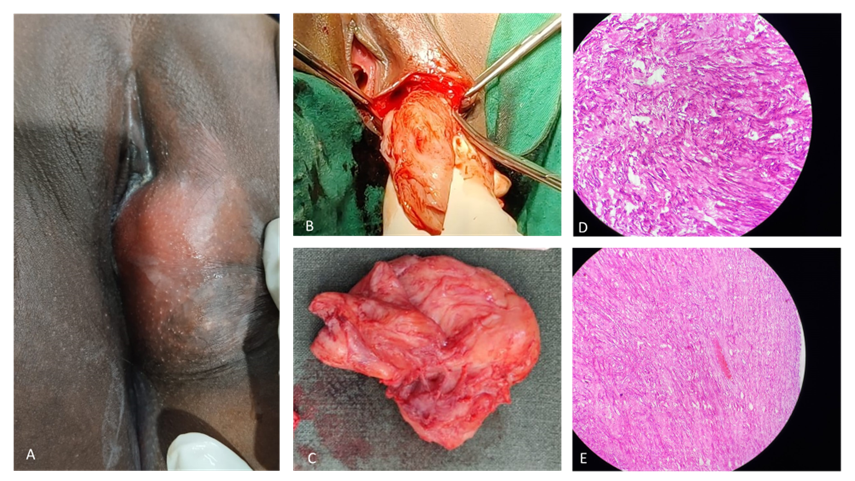
On examination a 4x5x3 cm mass arising from the left labium majus was noted. The mass was soft in consistency, non-tender, with no erythema, pushing the labia minora medially. Relevant investigations were done and noted to be normal. Transperineal ultrasound of the region showed well defined hypoechoic area in left lateral vulval region likely fibroma or fibrothecoma with a depth of about 4cm.
FNAC of the mass showed features suggestive of leiomyoma. Excision of the mass ([Figure 1] B) was done under anaesthesia and the dead space was obliterated by sutures.
Grossly, grey pink to grey white globular soft tissue mass measuring 5x4.5x2cm was noted. ([Figure 1] C) External surface was unremarkable. Cut section showed soft tumour with glistening surface.
Histopathology report showed spindle cells arranged in short fascicles, few scattered cells with eosinophilic cytoplasm, intervening stroma contained small to medium vessels with few ectatic blood vessels, interspersed collagen and occasional lymphocytes seen and no mitotic activity was seen. ([Figure 1] D and E)
Discussion
Angiofibroma of the vulva is a relatively rare benign stromal tumour seen in middle aged and older women. This was a rare case seen in a 20-year-old patient. Treatment consists of excision of the tumour. Ultrasound was done to know the size and depth of the tumour before excision. Patient was followed up and no recurrence was note in the left labium majus. Hence, malignancy and recurrence are rare.[6] Differential diagnoses that can be considered are - Bartholin’s cyst, lipoma, vulval cyst.
Phyllodes Tumour of Vulva
Phyllodes tumour (PT) is an uncommon fibroepithelial neoplasm of the breast.[7]
PTs are primarily found in the breast. But rare reports have been described arising in the vulva that may originate from anogenital mammary-type glands. These present typically as a unilateral painless mass, mostly involving labia majora, labia minora, or inter labial cleft. Histologically they show the features seen in the breast which are biphasic with bilayer epithelium and ductal hyperplasia and spindle celled stroma.[7]
Most cases are benign, but some maybe borderline or low potential malignant.[8]
Case report 2
A 45‑year‑old female presented with a vulvar mass in the left labium majus which was gradually increasing in size in the last one year and was painful since the last 15 days. Patient was P6L5A1. She had regular menstrual cycles and was a known case of hypertension in the last 1 year on treatment. Patient had no history of lump in breast and no history of hormonal therapy.
General physical examination was normal. Per abdomen - tubectomy scar. Local examination of the vulva showed a pedunculated mass arising from left side labium majus and measured 7x4.5x3cm. ([Figure 2]A) The mass was soft to firm in consistency, freely mobile, nodular and non-tender with a stalk of 4x2x1.5cm covered with hairy skin. Focal ulceration of 1cm of the overlying skin of the main lesion was noted which was covered with minimal slough. This vulvar mass and stalk were excised under short GA and sent for histopathological examination.
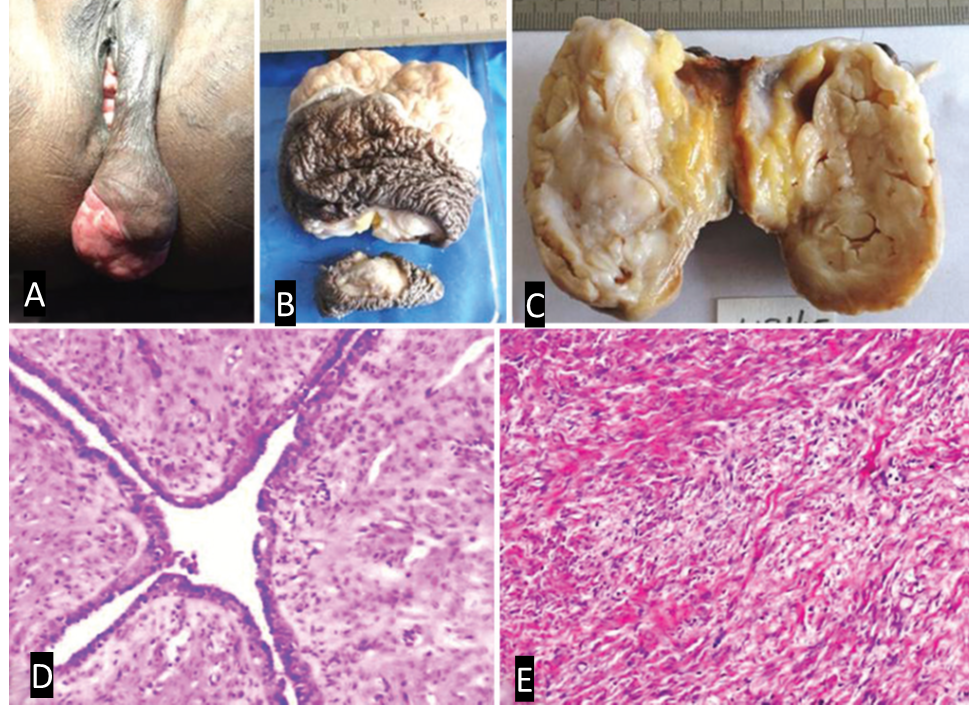
The cut surface was grey white, with slit like spaces, tiny cysts, mucoid and gelatinous areas. The tissue from the stalk of the main lesion was covered with hairy skin and measured 4.0x2.0x1.5 cm. ([Figure 2] B, C)
Histopathological examination of the cut section of the main lesion showed a neoplasm with spindle celled stroma with tapered nuclei in a collagenized background and biphasic morphology with intracanalicular pattern of slit like ducts with leaf like architecture. ([Figure 2] D, E) Ducts were lined by bilayered epithelium with inner cuboidal to columnar cells and outer basal cells. There was no cellular atypia and no mitoses seen in the stromal cells. The overlying skin showed an ulcer covered with inflammatory exudate.
Immunohistochemistry (IHC) of the tumour tissue was done which showed strong positivity for Progesterone Receptor (PR), Estrogen Receptor (ER) and Gross Cystic Disease Fluid Protein‑15 (GCDFP ‑15). A diagnosis of benign phyllodes tumour of the vulva was made by routine histopathology examination which was substantiated by IHC. Patient had no recurrence of the tumour on follow up for six years.
Discussion
Phyllodes tumour of breast comprises less than 1% of primary breast tumours and is diagnosed by typical leaf like architecture with biphasic pattern.[9] Proliferative breast lesions can be seen in extramammary sites such as vulva, anus, seminal vesicle, prostate and axilla.
The differential diagnosis of phyllodes tumour of the vulva includes other biphasic tumours such as fibroadenoma, papillary hidradenoma and chondroid syringoma.[10]
IHC markers specific for breast tumours are positive in phyllodes tumour of the vulva with the epithelial cells showing nuclear positivity for PR and ER. The other marker which is always positive in ducts with apocrine change is GCDFP‑15. Local recurrence is known with phyllodes tumour if not excised completely.[10]
PT of the vulva is a rare tumour with typical histopathology. Due to the uncommon site of occurrence – vulvar, IHC markers specific for mammary tissue is contributory for the diagnosis of the condition.
Hemangioma of Vulva
Hemangiomas are soft, proliferative tumours commonly situated in the cervico-facial region. Vulvar hemangiomas are rare which grow rapidly and might completely involute like a typical hemangioma noted at other sites.[11]
These occur as painless swellings on the vulva that increase in size gradually over time. The most common differential diagnoses are fibrolipoma and hamartoma.[11]
Case report 3
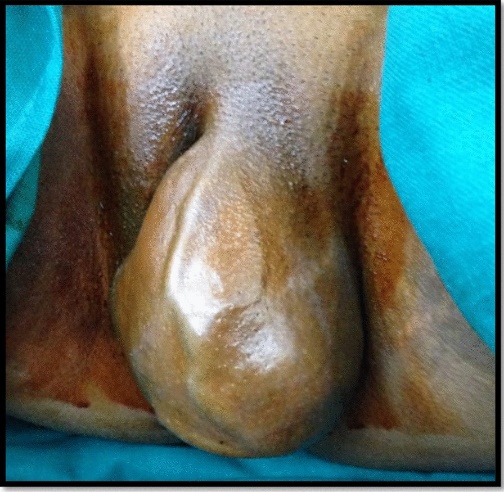
A 28-year-old patient presented with a vulvar mass. Patient came with complaints of swelling in the vulva – left labium majus. Initially small to start with and increased to the size of 5x6cm. It was of insidious onset, painless in nature. Patient was P2L2 with both vaginal deliveries. Patient had no significant past history, family history and personal history.
General physical examination was clinically normal. Local examination revealed a mass of 5x6cm, soft in consistency, non-tender in the left labium majus. (Figure 3) Patient underwent excision of the mass. Gross appearance - soft mass, and cut section showed features suggestive of lipoma.
Histopathological examination revealed cystically dilated tortuous blood vessels filled with red blood cells below the epidermis. No nuclear atypia noted. No abnormal mitotic activity noted. Histopathological examination confirmed features of cavernous hemangioma of the vulva.
Discussion
Vulvar hemangioma is a rare vascular tumour occurring at any age. These are mostly benign and treated by excision of the tumour.
Vulvar hemangiomas are rare and can be identified by Ultrasound or MRI to exclude other tumours like lipoma, angiokeratoma, hamartoma, lipoma and vascular malformations. Most of the lesions involute spontaneously with time. A course of corticosteroids may be tried to minimize the inflammatory process. Those lesions which are persistent and symptomatic and are causing discomfort to the patient, require surgical excision. Histopathological examination is necessary for confirmation of the diagnosis. Follow up is necessary for monitoring recurrence.[12]
Conclusion
Vulvar tumours are uncommon and mostly benign, typically diagnosed with ultrasound and confirmed via histopathology. The primary treatment is surgical excision. Follow-up is essential to monitor for recurrence or rare progression to malignancy. Recurrence rates vary: vulvar angiofibromas rarely recur, phyllodes tumours may recur if not fully removed, and hemangiomas have low recurrence post-treatment. Overall, these lesions are benign with malignancy being a rare occurrence.
Source of Funding
None.
Conflict of Interest
The authors declare no conflict of interest.
Anonymity and Consent
Patient anonymity was maintained and informed consent was taken for the data.
References
- VA Maldonado. Benign vulvar tumors. Best Pract Res Clin Obstet Gynaecol 2014. [Google Scholar]
- EM Messalli, ML D'Aponte, R Luise, L Rossiello, M Rotondi, PD Franciscis. An apparently benign vulvar mass: possibly a rare malignancy. Eur J Gynaecol Oncol 2012. [Google Scholar]
- JI Allbritton. Vulvar Neoplasms, Benign and Malignant. Obstet Gynecol Clin North Am 2017. [Google Scholar]
- M Khmou, N Lamalmi, A Malihy, L Rouas, Z Alhamany. Cellular angiofibroma of the vulva: a poorly known entity, a case report and literature review. BMC Clin Pathol 2016. [Google Scholar]
- JE Lane, AN Walker, EN Mullis, JG Etheridge. Cellular angiofibroma of the vulva. Gynecol Oncol 2001. [Google Scholar]
- VD Mandato, S Santagni, A Cavazza, L Aguzzoli, M Abrate, GBL Sala. Cellular angiofibroma in women: a review of the literature. Diagn Pathol 2015. [Google Scholar]
- S Somasegar, L Han, A Miller, P Wanjari, P Wang, JA Bennett. Phyllodes tumor of the vulva: A case report and literature review highlighting a novel manifestation of Cowden syndrome. Gynecol Oncol Rep 2021. [Google Scholar]
- A Kilitci, O Arıoz. Primary Benign Phyllodes Tumor of The Vulva: Case Report and Review of Literature. Eur J Breast Health 2019. [Google Scholar]
- K Venkatesh, T Jayanthy, S Patil. Benign phyllodes tumor of the vulva. Indian J Pathol Microbiol 2021. [Google Scholar]
- DV Kazakov, DV Spagnolo, CJ Stewart, J Thompson, A Agaimy, G Magro. Fibroadenoma and phyllodes tumors of anogenital mammary-like glands: a series of 13 neoplasms in 12 cases, including mammary-type juvenile fibroadenoma, fibroadenoma with lactation changes, and neurofibromatosis-associated pseudoangiomatous stromal hyperplasia with multinucleated giant cells. Am J Surg Pathol 2010. [Google Scholar]
- A Verma, G Sharma, N Srivastava, N Verma. An unusual presentation of vulvar cavernous hemangioma in a 10-year-old premenarchal girl: a rare entity. Int J Reprod Contracept Obstet Gynecol 2023. [Google Scholar]
- JMD Silva, ER Calife, JCDS Cabral, Hpf Andrade, A K Gonçalves. Vulvar Hemangioma: Case Report. Rev Bras Ginecol Obstet 2018. [Google Scholar]
