- Visibility 253 Views
- Downloads 29 Downloads
- DOI 10.18231/j.ijogr.2023.001
-
CrossMark
- Citation
A review on the impact of analgesic use during pregnancy on stillbirth
- Author Details:
-
Girish B S *
-
Joel M Johns
-
Meghana C S
-
Rakshitha H R
-
Vineela Nekkanti
Introduction
World Health Organization (WHO) defines stillbirth as foetal death after 28 weeks of pregnancy, but before or during birth.[1] Stillbirth is a tragic complication of the pregnancy which is associated with emotional, social and economic disturbances which is crucial to address the issue prior and to assess at each step of the pregnancy to avoid this complication.
Stillbirth can be a result of many causes like obesity, smoking, advanced maternal age (over 40), multiparity, hypertensive disorders of pregnancy (HDP), gestational diabetes, some ethnic race especially black women (because of no proper perinatal care) and others like inappropriate gestational periods, infections, thrombophilia etc.[2], [3], [4], [5], [6], [7], [8] But in recent years’ usage of drugs in pregnancy has been increased dramatically, globally it is estimated that 23%–85% of women use one or more types of prescribed medications during pregnancy.[9], [10] Prior to a new medicine being released into the market, the company seldom ever conducts studies on pregnant mothers to ascertain the drug's effects on the foetus.[11] As a result, safety profile for most of the drugs are poorly established.
The most recent statistics showed that there were 13.9 stillbirths per 1,000 live births worldwide in 2019.[12] This translates to one stillborn child every 16 seconds, or one in every 72 births overall. However, given that stillbirths are frequently underreported, this figure may be misinterpreted. The perinatal mortality rate in India currently is 36 deaths per 1,000 pregnancies.[13] According to Government’s Annual report on the registration of Birth and Death reports act, 1969 stated that, in Karnataka 3.48% is the stillbirth rate in 2020.[14] In order to alleviate the burden of stillbirth, Government of India initiated 'The India Newborn Action Plan' in 2014, with the goal of lowering the rate of stillbirth by one-third nearing to 2025.[15]
As a thumb rule, each prescription has its own set of advantages and hazards, which may directly or indirectly affect the foetal health. Drugs like anticancer drugs, antiepileptic drugs, antipsychotics, analgesics cause stillbirth. In general, drug exposure was associated with the two-fold increased risk of stillbirth in pregnancy.[16] Usage of OTC during pregnancy has been increased,[17] which risks the foetus health. Painkillers are often used to self-medicate without the supervision of a medical professional.[18] In the current review, the risk of stillbirth on usage of analgesics during pregnancy is underlined.
Discussion
Factors influencing the risk of stillbirth:
Stillbirth can be caused by a variety of factors, which account for foeto-maternal mortality; nevertheless, documenting the reason for stillbirth is a stumbling block that leads to the notion that the cause of stillbirth is unclear.[19] Some of the factors are discussed hereafter.
Advanced maternal age
In most industrialized nations, the average mother age during delivery has increased in recent decades.[20] The risk of stillbirth during pregnancy is three times higher in women of advanced maternal age i.e. beyond the age of 40, with or without any medical issues.[21] The combination of age and gestational week results in strain on expectant mothers. Conventionally, stillbirth rates are high during the early gestational week (20-23 weeks), decline between 39 and 41 weeks of gestation and then subsequently rises at 42 weeks and beyond.[22]
Studies showed that placental abnormal phenotype was prevalent in women aged 40 and above, in addition to the reduction in food intake that comes 8with aging in women. Ageing is also related with increased risk of elevated reactive oxygen species, inflammatory markers that cause oxidative stress, and tissue functio laesa that may be a factor in placental abnormalities, which exhibits as increased placental weight, altered utero-placental vascular function and decreased placental efficiency attributing to increased risk of stillbirth.[23]
Obesity
Women who are pregnant should look for both themselves and the developing foetus. High Body Mass Index (BMI) adds significantly to any medical problem; bearing a child will be a health burden for those with excessive body mass. Obesity defined as BMI > 30kg/m2, doubles the chance of stillbirth.[24] Corpulence increases the length of the umbilical cord accounting to hyper coiling, which increases the risk of cord entanglement, clogging of the umbilical cord, and umbilical knot around the foetus, reducing the blood flow and resulting in placental insufficiency, which causes foetal growth restriction and stillbirth.[25]
Increased BMI may be a result of inheritance or a sedentary lifestyle. In order to minimize stillbirth, pregnant women should maintain a good height to body weight ratio.
Social habits
Physical and emotional stress along with lack of education and social awareness would make one dependent on social vices like chewing tobacco, smoking and drinking alcohol.
Smoking and chewing tobacco increases the incidence of stillbirth by 14% and has its own impact on the health of the mother and developing foetus before, after, and even during pregnancy.[26], [27] Cigarette smoking and alcohol consumption causes narrowing of placental vessels and consequently impairing blood supply to foetus, in addition to this, reduces foetal oxygenation causing complex cascade resulting in shock and foetal death.[26], [28]
Socio-economic status
According to National Institute for Transforming India (NITI) Aayog, 25.01% of India’s population are considered as multidimensionally poor in 2021,[29] which contributes to one-fourth of Indian population suggesting lack of education, awareness, poor antenatal care contributing to majority of pregnancy-related complications. A comprehensive evaluation of research from developing nations found that poor socioeconomic position of pregnant women was strongly related with stillbirth, with an attributable percentage ranging from 2% to 75% of the population.[30] In addition to all these, lack of woman’s autonomy in terms of decision making may majorly affect the health of the mother and foetus contributing to maternal and foetal complications including stillbirth.[31]
Comorbidities
Age, low educational attainment, and socioeconomic standing all have an effect on an individual's overall health, leading to several chronic conditions that can end in miscarriage.
Hypertensive disorders of pregnancy (HDP) like preeclampsia and eclampsia have resulted in 15% of perinatal foetal mortality, similarly pre-gestational diabetes and Gestational diabetes mellitus increases the risk of stillbirth by 4-5 folds by causing foetal anaerobic respiration, shock and death. India being the World Diabetes Capital, Indian pregnant women are at high risk of stillbirth.[32], [33], [34], [35], [36] In addition to this, anaemia by default reduces placental oxygenation resulting in hypoxic environment attributing to stillbirth.[37]
Conditions like Polycystic Ovarian Disorder (PCOD), Placenta Previa, Abruptio Placentae, oligohydramnios, infections etc causes morphological or pathological changes leading to malformed placenta which results in abnormal implantation, foetal growth restriction, placental insufficiency, necrotic placenta contributing to stillbirth.[38], [39], [40], [41]
Drug use during pregnancy
Pregnancy is a unique physiological and psychological state, where the pharmacology of drugs is affected by changes in body physiology throughout time, which is of primary concern.[42] Some of the drugs can cross placenta and reach developing foetus which can cause potential harm due to physiological adaptation in pregnant women. The drugs, by default, possesses inbuilt harm in pregnancy which was witnessed by the thalidomide and diethylstilboestrol catastrophe.[43] These tragedies have led to more serious concerns, the Food and Drug Administration (FDA) established stringent norms on the use of drugs during pregnancy. Thereby, FDA classifies the drugs based on their teratogenic activity.[42]
|
Categories |
Description |
Example |
|
A |
Adequate studies on pregnant women indicated no foetal risk |
Vitamin B, C, D, E and folic acid, thyroxin etc. |
|
B |
Animal studies have showed no evidence of harm to the foetus, but lack of studies in pregnant women |
Acetaminophen, Phenacetin etc. |
|
C |
Animal studies have shown adverse effect or no animal studies are conducted and no adequate studies in pregnant women |
Aspirin, Gentamicin, antimalarial etc. |
|
D |
Studies showed risk to foetus, but benefit may outweigh the risk |
Streptomycin, Tetracycline etc. |
|
X |
Studies showed evident risk to the foetus and use of the drug is contraindicated in pregnant women. |
Estrogen, Norethindrone Etc. |
Some women become pregnant with pre-existing medical issues and few others develop novel medical conditions during the course of pregnancy that necessitate therapeutic intervention. Failure to address these issues has an impact on the health of both the expectant mother and the growing baby.[44] According to a study conducted by Sharma R and co-authors, around 8% of awaiting mothers require therapeutic intervention because of prevailing medical issues and pregnancy-related complications.[45] Considering the mother and foetal health; vitamins, minerals, iron and other dietary supplements are essential.
Drug use during pregnancy plays a pivotal role in ameliorating the mother's health and well being; nevertheless, for drug used to be successful, it must be non-toxic, effective, and should be rationally used. Primary factors of irrational medication usage include ease of access, feelings of improvement, underestimation of drug toxicity, unethical advertising, cost-driven attitude, incorrect perceptions of drug side effects, lack of adequate drug education by the prescriber, a lack of regulatory control system, etc.[46] The outcome of irrational use of drugs is exhibited as maternal and foetal complications owing to maternal as well as foetal death.
As cited previously, the safety of pharmaceuticals in pregnancy is not well established, and data indicates that Over-The-Counter (OTC) and prescription drug usage is widespread throughout pregnancy, with 2-3% of drug use resulting in birth abnormalities.[42] OTC medications are cheap, provide accentuated symptomatic relief which makes a pregnant woman to rely on OTC, thus promoting self-medication without being aware of risk. This had promoted pregnant women to go beyond OTC range that includes ‘Schedule H’ drugs being dispensed irrationally which are categorised under prescription drugs.[47], [48] The majority of antibiotics belong within the schedule H group of medications that are arbitrarily prescribed and used during pregnancy which could attack the mother's host cells, endangering her health and forcing her to ingest more and more drugs, perhaps leading to stillbirth.
Pregnancy-related irrational medication use has grown in developing nations like India as a result of drug dispensing without a prescription, distributing by non-pharmacists, and dispensing through a third party.[49] Analgesics, antipyretics, cough and nasal decongestants, antihistamines, and other drugs are available over-the-counter. Antibiotics, opioid analgesics, antihypertensive, antianginal, antipsychotic, and other medications on prescription are included.
Drug use during pregnancy will have an impact on the foetus, either directly or indirectly, causing harm, aberrant development, and even death. They also impair the placental function by causing placental insufficiency, and few results in preterm uterine contraction injuring the foetus contributing to various pregnancy-related complications including stillbirth.[42]
Analgesic use in pregnancy
Many circumstances might drive a pregnant woman to use analgesics; for example, drastic changes in human physiology during pregnancy produce discomfort, which is majorly perceived as pain.

Non-opioid analgesics include Non-Steroidal Anti-Inflammatory Drugs (NSAIDS), such as aspirin, ibuprofen, diclofenac, and naproxen, as well as paracetamol. These analgesics are available over-the-counter, allowing easy access owing to arbitrary use. Due to unavoidable stressful commitments, pregnant women frequently use a lot of over-the-counter painkillers to manage their discomfort, unknowingly endangering the unborn child's health. To minimise pregnancy-related issues, the use of NSAIDS as analgesics is not suggested in pregnancy unless required and prescribed by a medical practitioner, and should be avoided beyond the gestational age of 30 weeks. While certain analgesics, such as acetaminophen (paracetamol), are safe to take throughout pregnancy.[50]
In the US, 2-4% of pregnancies involved at least one opioid analgesic for pain, making the use of opioids during pregnancy a severe health risk.[51] Opioids are renowned for their teratogenic effects, which pose serious health risks to both the mother and the foetus and result in issues with pregnancy. Morphine, pethidine, codeine, methadone, buprenorphine, and fentanyl are few examples of opioid analgesics.[51]
Mechanism of analgesics causing stillbirth
Non-opioid analgesic
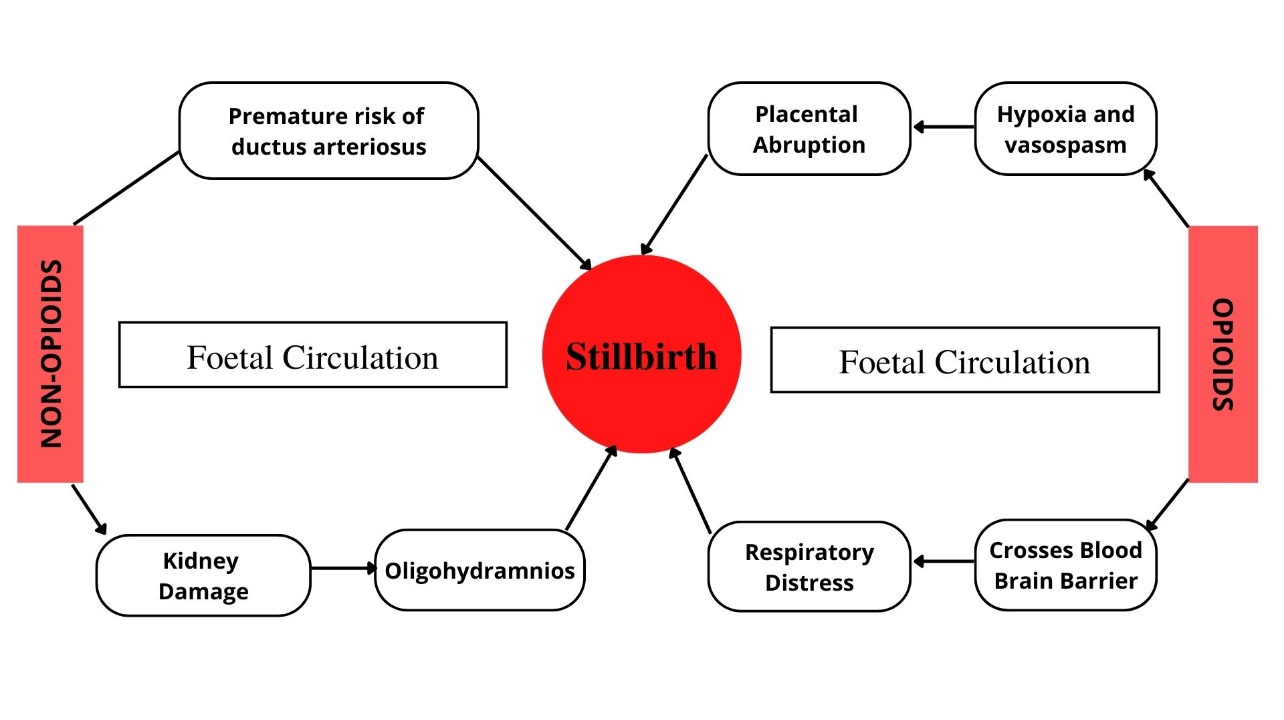
During pregnancy, the increased plasma volume, cardiac output and glomerular filtration rate changes the pattern of drug absorption, thus increasing the bioavailability of free drug flowing in the circulation of mother with features of lipid solubility and low molecular weight making it simple for these free drugs to cross the placenta allowing the entry into foetal circulation which exhibits some hazardous effects. Drugs that belongs to the above category are aspirin, ibuprofen, naproxen and acetaminophen.[52]
NSAIDs are cyclooxygenase enzyme inhibitors that are widely used by 19% of the population for their analgesic, antipyretic, and anti-inflammatory properties. NSAIDS are often used in the first trimester and are generally avoided in the third trimester owing to adverse effects.[53]
The last three months of pregnancy are the most susceptible period, as the body gradually adapts to the change as the foetus develops. NSAIDS easily pass through the placenta, and inhibition of prostanoid action may result in miscarriage. After passing through the placental barrier, they enter the foetal circulation, causing kidney injury since the developing kidneys are unable to handle the foreign substance. This causes the placenta to have very little amniotic fluid, which leads to oligohydramnios, which can cause 2 cord injuries and foetal mortality due to insufficient nutritional supply.[54] ([Figure 2]) According a cohort study conducted by Aikaterini Zafeiri et al., on singleton pregnancies showed 405 stillbirths out of 43998 pregnant women who have consumed at least one over-the-counter analgesics.[50]
Opioid analgesic
Opioid use during pregnancy has been connected to a number of obstetric and perinatal problems. Pregnancies exposed to prenatal opioid in the first and second trimesters have an increased risk of stillbirth.[51] The biggest danger with opioid usage is dependency, and most women hide their opioid use for a variety of reasons, one of which is a sense of improvement. In the idea of opioid analgesics, the debate between "usage" and "abuse" persists.
When opioids are taken during pregnancy, they penetrate the placenta and enter the growing foetus's system, where they pass the blood brain barrier, causing respiratory distress, foetal growth limitation, and foetal death.[55] On the other hand, it also results in placental abruption by causing hypoxia and vasoconstriction of placental bed. Some of the opioid like cocaine can result in early uterine contraction leading to foetal injury and death.[56] A study conducted by Brogly et al. showed a statistically significant association between the occurrence of stillbirth and opioid exposure.[51]
Conclusion
Analgesics are usually blindfolded as safe for the use during pregnancy, but they do carry potential risk such as stillbirth, especially with the use in the second and third trimester. The irrational use of analgesics during pregnancy is high in India without the knowledge of risk attributed by the drugs. Hence, it is of paramount importance to promote the rational usage of analgesics, which can be attained either by educating the pregnant woman about foetal risks and/or by employing a registered pharmacist who can ensure dispensing of analgesics with prior medical authorization.
Source of Funding
None.
Conflict of Interest
None.
References
- . Stillbirth [Internet]. . [Google Scholar]
- S Carmichael, Y Blumenfeld, J Mayo, E Wei, J Gould, D Stevenson. Prepregnancy Obesity and Risks of Stillbirth. PLoS One 2015. [Google Scholar]
- E Raymond, S Cnattingius, JL Kiely. Effects of maternal age, parity, and smoking on the risk of stillbirth. Br J Obstet Gynaecol 1994. [Google Scholar]
- TA Mills, T Lavender. Advanced maternal age. Obstet Gynaecol Reprod Medi 2011. [Google Scholar]
- R Fretts. Stillbirth Epidemiology, Risk Factors, and Opportunities for Stillbirth Prevention. Clin Obstet Gynecol 2010. [Google Scholar]
- KJ Gibbins, RM Silver, H Pinar, UM Reddy, CB Parker, V Thorsten. Stillbirth, hypertensive disorders of pregnancy, and placental pathology. Placenta 2016. [Google Scholar]
- R Starikov, D Dudley, UM Reddy. Stillbirth in the pregnancy complicated by diabetes. Curr Diab Rep 2015. [Google Scholar]
- G Smith, R Fretts. Stillbirth. Lancet 2007. [Google Scholar]
- M Gendron, B Martin, D Oraichi, A Bérard. Health Care Providers’ Requests To Teratogen Information Services On Medication Use During Pregnancy And Lactation. Eur J Clin Pharmacol 2009. [Google Scholar]
- A Mitchell, S Gilboa, M Werler, K Kelley, C Louik, S Hernández-Díaz. Medication use during pregnancy, with particular focus on prescription drugs: 1976-2008. Am J Obstet Gynecol 2011. [Google Scholar]
- G Koren, A Pastuszak, S Ito. Drugs In Pregnancy. N Engl J Med 1998. [Google Scholar]
- . Stillbirths and stillbirth rates - UNICEF DATA [Internet]. . [Google Scholar]
- . Health and Family Welfare Statistics in India 2019-20 [Internet]. 2021. [Google Scholar]
- . Annual Report on the Registration of Births and Deaths act, 1969 [Internet]. Government of Karnataka, 2020. . [Google Scholar]
- M Roy. Mitigating The Stillbirth Challenge In India. Lancet 2016. [Google Scholar]
- E Sevene, A Bardají, A Mariano, S Machevo, E Ayala, B Sigaúque. Drug Exposure And Pregnancy Outcome In Mozambique. Pediatric Drugs 2012. [Google Scholar]
- A Lupattelli, O Spigset, M Twigg, K Zagorodnikova, A Mårdby, M Moretti. Medication use in pregnancy: a cross-sectional, multinational web-based study. BMJ Open 2014. [Google Scholar]
- S Hultzsch, W Paulus, S Padberg, A Fietz, C Schaefer, K Dathe. First trimester naproxen exposure and outcome of pregnancy - A German case series. Reprod Toxicol 2021. [Google Scholar]
- S Cnattingius, O Stephansson. The epidemiology of stillbirth. Semin Perinatol 2002. [Google Scholar]
- L Huang, R Sauve, N Birkett, D Fergusson, CV Walraven. Maternal Age And Risk Of Stillbirth: A Systematic Review. CMAJ 2008. [Google Scholar]
- UM Reddy, CW Ko, M Willinger. Maternal Age And The Risk Of Stillbirth Throughout Pregnancy In The United States. Am J Obstet Gynecol 2006. [Google Scholar]
- MF Macdorman, UM Reddy, RM Silver. Trends in Stillbirth by Gestational Age in the United States, 2006-2012. Obstet Gynecol 2006. [Google Scholar]
- SC Lean, AEP Heazell, MR Dilworth, TA Mills, RL Jones. Placental Dysfunction Underlies Increased Risk Of Fetal Growth Restriction And Stillbirth In Advanced Maternal Age Women. Sci Rep 2017. [Google Scholar]
- N Penn, E Oteng-Ntim, L Oakley, P Doyle. Ethnic variation in stillbirth risk and the role of maternal obesity: analysis of routine data from a London maternity unit. BMC Pregnancy Childbirth 2014. [Google Scholar]
- H Åmark, M Westgren, M Sirotkina, I Hulthén Varli, M Persson, N Papadogiannakis. Maternal obesity and stillbirth at term; placental pathology-A case control study. PLoS One 2021. [Google Scholar]
- T Marufu, A Ahankari, T Coleman, S Lewis. Maternal smoking and the risk of still birth: systematic review and meta-analysis. BMC Public Health 2015. [Google Scholar]
- P Gupta, S Subramoney. Smokeless Tobacco Use And Risk Of Stillbirth. Epidemiology 2006. [Google Scholar]
- L Burd, D Roberts, M Olson, H Odendaal. Ethanol And The Placenta: A Review. The Journal of Maternal-Fetal &. Neonatal Medicine 2007. [Google Scholar]
- . National Multidimensional Poverty Index Baseline Report Based on NFHS-4 (2021) [Internet]. 2021. [Google Scholar]
- E Mcclure, S Saleem, O Pasha, RL Goldenberg. Stillbirth in developing countries: a review of causes, risk factors and prevention strategies. J Matern Fetal Neonatal Med 2009. [Google Scholar]
- L Sanneving, N Trygg, D Saxena, D Mavalankar, S Thomsen. Inequity In India: The Case Of Maternal And Reproductive Health. Global Health Action 2013. [Google Scholar]
- M Basta, K Hanif, S Zafar, A Khabazeh, F Amin, SS Khan. Impact of Hypertensive Disorders of Pregnancy on Stillbirth and Other Perinatal Outcomes: A Multi-Center Retrospective Study. Cureus 2022. [Google Scholar]
- S Mackin, S Nelson, J Kerssens, R Wood, S Wild. Diabetes and pregnancy: national trends over a 15 year period. Diabetologia 2018. [Google Scholar]
- SK Pandey, V Sharma. Battling The Emerging Epidemic Of Diabetic Retinopathy. Indian J Ophthalmol 2018. [Google Scholar]
- T Stacey, P Tennant, L Mccowan, E Mitchell, J Budd. Gestational diabetes and the risk of late stillbirth: a case-control study from England, UK. BJOG 2019. [Google Scholar]
- DJ Dudley. Diabetic-associated stillbirth: incidence, pathophysiology, and prevention. Obstet Gynecol Clin North Am 2007. [Google Scholar]
- M Nair, M Knight, S Robinson, C Nelson-Piercy, S Stanworth, D Churchill. Pathways of association between maternal haemoglobin and stillbirth: path-analysis of maternity data from two hospitals in England. BMJ Open 2018. [Google Scholar]
- H Valgeirsdottir, T Kunovac Kallak, I Sundström Poromaa, M Jonsson, N Roos, L Lindström. Polycystic ovary syndrome and risk of stillbirth: a nationwide register-based study. BJOG 2021. [Google Scholar]
- A Yeniel, A Ergenoglu, I Itil, N Askar, R Meseri. Effect of placenta previa on fetal growth restriction and stillbirth. Arch Gynecol Obstet 2012. [Google Scholar]
- CV Ananth, GS Berkowitz, DA Savitz, RH Lapinski. Placental Abruption And Adverse Perinatal Outcomes. JAMA 1999. [Google Scholar]
- L Figueroa, E Mcclure, J Swanson, R Nathan, A Garces, J Moore. Oligohydramnios: a prospective study of fetal, neonatal and maternal outcomes in low-middle income countries. Reprod Health 2020. [Google Scholar]
- P Sachdeva, BG Patel, BK Patel. Drug Use In Pregnancy; A Point To Ponder!. Indian J Pharm Sci 2009. [Google Scholar]
- M W Melton. Take two Aspirin or not? Risk of medication use during pregnancy. Mother Baby J 1999. [Google Scholar]
- SE Andrade, JH Gurwitz, RL Davis, KA Chan, JA Finkelstein, K Fortman. Prescription drug use in pregnancy. Am J Obstet Gynaecol 2004. [Google Scholar]
- R Sharma, B Kapoor, U Verma. Drug utilization pattern during pregnancy in North India. Indian J Med Sci 2006. [Google Scholar]
- M Vance, W Millington. Principles of irrational drug therapy. Int J Health Serv 1986. [Google Scholar]
- G Shruti, PK Sree, YV Rao. Drug use pattern of over-the-counter and alternative medications in pregnancy: A cross sectional descriptive study. Natl J Physiol, Pharm Pharmacol 2015. [Google Scholar]
- S Kamat, P Marathe, R Tripathi, S Raut, N Khatri. Over-The-Counter Medicines: Global Perspective And Indian Scenario. J Postgrad Med 2020. [Google Scholar]
- G Porter, N Grills. Medication Misuse In India: A Major Public Health Issue In India. J Public Health (Oxf) 2016. [Google Scholar]
- A Zafeiri, EA Raja, RT Mitchell, DC Hay, S Bhattacharya, PA Fowler. Maternal over-the-counter analgesics use during pregnancy and adverse perinatal outcomes: cohort study of 151 141 singleton pregnancies. BMJ Open 2022. [Google Scholar]
- S Brogly, M Velez, M Werler, W Li, A Camden, A Guttmann. Prenatal Opioid Analgesics and the Risk of Adverse Birth Outcomes. Epidemiology 2021. [Google Scholar]
- J Kwok, E Luedecke, H Hall, A Murray, B Auyeung. Analgesic drug use in pregnancy and neurodevelopment outcomes: an umbrella review. Neurosci Biobehav Rev 2022. [Google Scholar]
- MV Gelder, N Roeleveld, H Nordeng. Exposure to non-steroidal anti-inflammatory drugs during pregnancy and the risk of selected birth defects: a prospective cohort study. PLoS One 2011. [Google Scholar]
- . FDA warns of possible fetal risk linked to NSAIDs [Internet]. . [Google Scholar]
- HS Fricker, S Segal. Narcotic Addiction, Pregnancy, and the Newborn. Adolesc Med 1978. [Google Scholar]
- J Zipursky, D Juurlink. Opioid use in pregnancy: An emerging health crisis. Obstetric Medicine 2020. [Google Scholar]
How to Cite This Article
Vancouver
S GB, Johns JM, S MC, R RH, Nekkanti V. A review on the impact of analgesic use during pregnancy on stillbirth [Internet]. Indian J Obstet Gynecol Res. 2025 [cited 2025 Sep 09];10(1):1-6. Available from: https://doi.org/10.18231/j.ijogr.2023.001
APA
S, G. B., Johns, J. M., S, M. C., R, R. H., Nekkanti, V. (2025). A review on the impact of analgesic use during pregnancy on stillbirth. Indian J Obstet Gynecol Res, 10(1), 1-6. https://doi.org/10.18231/j.ijogr.2023.001
MLA
S, Girish B, Johns, Joel M, S, Meghana C, R, Rakshitha H, Nekkanti, Vineela. "A review on the impact of analgesic use during pregnancy on stillbirth." Indian J Obstet Gynecol Res, vol. 10, no. 1, 2025, pp. 1-6. https://doi.org/10.18231/j.ijogr.2023.001
Chicago
S, G. B., Johns, J. M., S, M. C., R, R. H., Nekkanti, V.. "A review on the impact of analgesic use during pregnancy on stillbirth." Indian J Obstet Gynecol Res 10, no. 1 (2025): 1-6. https://doi.org/10.18231/j.ijogr.2023.001
