- Visibility 1.5k Views
- Downloads 102 Downloads
- Permissions
- DOI 10.18231/j.ijogr.2025.016
-
CrossMark
- Citation
Monocryl 3-0 subcuticular in abdominal skin closure in cesarean sections
Abstract
Background: Cesarean sections are amongst the most commonly performed abdominal operations in women worldwide. Wound healing is an important factor for lower complication rate and patient satisfaction. Despite conflicting results, closure with subcuticular suture materials was found to be more advantageous considering wound healing, better cosmetic results and patient satisfaction rates.
Objectives: 1. To assess pain on 5th postoperative day. 2. To assess wound complications. 3. To assess scar at 6th week of follow up.
Materials and Methods: Observational study was conducted on cases admitted in obstetric department undergoing caesarean section from January 2023 to March 2024. Subcutaneous tissue was closed with interrupted sutures (PLAIN CATGUT 2-0) where subcutaneous tissue was >1cm thickness. Monocryl 3-0 subcuticular was used as an absorbable material for skin closure. Wound evaluations were performed during follow-up at 6th week by interviewing patients and local examination of wound.
Results: 75 cases were enrolled out of which 12 lost to follow up. The mean age was 27.40 ± 3.795 years. The mean BMI was 21.492 +-3.987 Kg/m2. Mean time for skin closure was 4.96± 1.382 mins. Mean pain score at post-operative day 5 was 5.05+1.451. 13 (8.7%) cases had mild pain, 57(38%) had moderate pain and 5(3.3%) had severe pain. At 6 weeks of follow up seroma was present in 9(6%) cases, 5 (3.3%) had infection, 5 (3.3%) had dehiscence 3 (2%) had hypertrophic scar and hematoma in only 2 (1.3%) cases. POSAS score was used for cosmetic scar assessment. Mean patient scar score was 6.128 ±1.291 and observer scar score was 6.173+-2.891.
Conclusion: Future research is needed on multicentric levels with extended follow-up periods and employing standardized, objective outcome measures to enhance the reliability and generalizability of findings across diverse patient populations.
Introduction
Caesarean section stands as one of the most frequently performed abdominal surgeries among women across the globe. The practice of suturing has ancient roots, dating back to at least 600 BC as evidenced in texts such as Susruta Samhitha. This historical text mentions suture materials derived from animal sinews, braided horsehair, leather strips and vegetable fibers. Furthermore, it provides detailed description of various types of needles, including triangular, round-bodied, curved, and straight needles.[1]
Various surgical approaches are employed for different aspects of the caesarean section procedure. However, many of these techniques lack thorough evaluation through randomized controlled trials, leaving uncertainty regarding their efficacy.[2] Many different suture materials and techniques had been explored before chromic catgut became the standard, which was at the end of 19th century. Many different suture materials such as Gold, silver and steel wire, animal and human hair, gut strings from sheep and goat, linin, silk had been used previously. At the beginning of 21st century various alternative products had been developed. Synthetic absorbable suture materials were introduced that surpassed catgut, basically in Europe. These materials elicit less tissue reactions thus promoting faster wound healing and strength. Nevertheless, catgut continued to have major role in wound care worldwide. The choice of an appropriate suture material for any wound closure largely contributes to the final functional and cosmetic outcome.[3]
A perfect suture would possess the following properties[4]
Adequate strength needed for tissue healing
Minimal tissue reactivity
Good handling characteristics
Resistant to bacterial growth and easy sterilization
Nonallergenic and noncarcinogenic
In the early 1970s, synthetic absorbable sutures were initially introduced by suture manufacturers in a braided configuration, utilizing materials such as polyglycolide (Dexon, Davis & Geck) or copolymers of glycolide and lactide (Vicryl, Ethicon). Conversely, barbed sutures have shown time reduction for dermal and epidermal skin closure along with overall operative time without raising concerns about blood loss or maternal complications.[5] Subsequently, in the 1980s, they introduced new polymers for use in monofilament sutures to overcome issues of tissue friction and infection rates associated with braided sutures.[6]
Monofilament suture is made up of a single strand, making it relatively resistant to harbour microorganisms. They offer lower tissue drag during placement, minimizing trauma to tissues, and reducing the risk of suture marks. They are ideal for procedures requiring fine tissue approximation and where tissue reactivity is a concern. They cause less tissue trauma during insertion and removal, making them suitable for delicate tissues hence reducing the risk of complications. When compared to multifilament sutures, monofilament sutures encounter less resistance when passing through tissue. However, caution is necessary during tying and handling of monofilament sutures to avoid crimping or crushing, which can weaken or nick the suture, leading to premature failure.
The first absorbable synthetic monofilament suture, PDS, a homopolymer of p-dioxanone, was introduced by Ethicon in 1984 (Somerville, NJ, USA). It alleviated some concerns that were associated with the use of braided sutures. PDS II, an improved version, was later introduced by Ethicon.[7] Although various absorbable monofilaments have been introduced since then, existing monofilament absorbable sutures generally do not have handling as good as braided sutures and often require more knots for secure closure.
Monocryl (Poliglecaprone)
Monocryl suture, composed of monofilament synthetic polymer, is known for the smooth surface, which reduces trauma to tissues and minimizes the risk of infection. This characteristic makes them particularly suitable for delicate tissues in obstetric and gynaecologic procedures, where minimizing tissue reaction and promoting wound healing are critical. Monocryl sutures provide superior handling characteristics due to the monofilament structure, allowing for easier tissue passage and knot tying. They are often preferred for fine tissue approximation and suturing in confined spaces, common in gynecologic surgeries. Monocryl sutures may have a relatively higher upfront cost compared to Prolene sutures, primarily due to manufacturing processes. However, need for suture removal is eliminated by their absorbable nature, potentially reducing overall procedure costs and patient discomfort. Prolene sutures, while more affordable initially, may incur additional costs associated with suture removal procedures.[8]
Controversy surrounds the optimal method for skin closure following cesarean delivery. Prior meta-analyses indicate that absorbable sutures decrease the risk of skin separation compared to staple sutures, albeit at the expense of increased wound closure time. Keeping in mind the ever evolving concept of perfect sutute material and technique for caesarean skin closure, Monocryl 3-0 subcuticular has been used for skin closure during caesarean and its cosmetic aspects and wound complications have been studied in the current study.
Materials and Methods
Place of study
Department of obstetrics and gynaecology at tertiary care hospital, Amritsar.
Study design
Observational study.
Study period
This study was conducted from 1st January 2023 to 31st March 2024.
Inclusion criteria
Patients undergoing caesarean section by pfannenstiel skin incision admitted in Department of Obstetrics and Gynaecology at Tertiary care hospital, Amritsar after applying exclusion criteria.
Exclusion criteria
Patients referred from outside in emergency.
Patients with undergoing vertical skin incision in present caesarean and with vertical skin incision in past.
Morbidly obese patients BMI>40.
Patients with previous history of wound complications
Patients with uncontrolled diabetes.
Patients with coagulation defects, hemodynamic instability, septicaemia or chorioamnionitis, on steroid or other immunosuppressant will be excluded.
Patients with gynaecological malignancies such as Ca ovaries, endometrium, cervix.
Patients with two or more gynaecological or obstetric surgeries in past
Patient with PROM or PPROM >12 hours in duration.
The study was conducted on patients, admitted in Obstetric department undergoing caesarean section. All the patients undergoing elective caesarean sections who met the inclusion criteria were included in the study. Detailed history was recorded including complete demographic details, dietary history, antenatal history, gynaecological history, past medical/surgical history, any previous antenatal complications.
Skin of all the patients was cleaned with povidone iodine 3 to 4 minutes before the operation started. Prophylactic antibiotic was given to all patients before operation. The pfannenstiel technique was used for all patients. Subcutaneous tissues was closed with interrupted sutures (Plain catgut 2-0) in case of more than 1 cm subcutaneous tissue thickness. Monocryl 3-0 was used as absorbable suture material for skin closure in randomly allocated patients. Time for skin closure was recorded in all patients.
Postoperative pain assessment using pain score on numerical rating scale ([Figure 1]) (NRS)[9] was done on fifth day post caesarean.
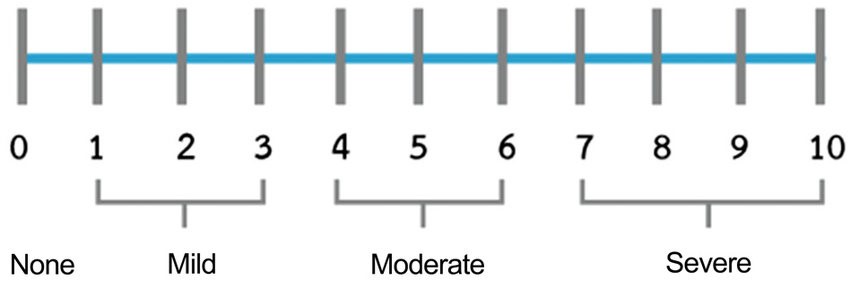
The patients were asked to make three pain ratings, corresponding to current, best and worst pain experienced over the past 24 hours. The average of these 3 ratings was used to represent the patient’s level of pain over the previous 24 hours.
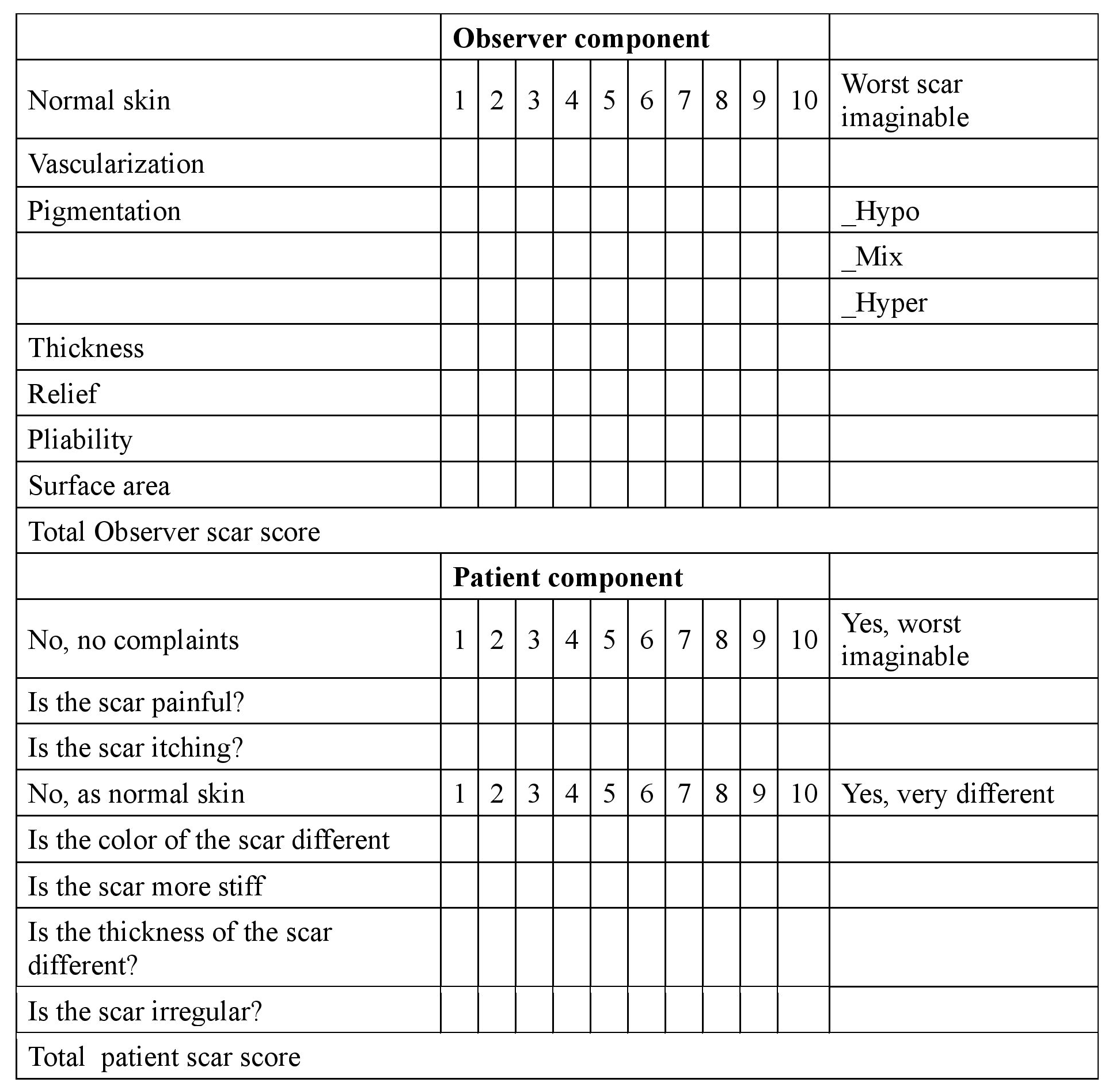
Antiseptic dressings were changed on fifth postoperative day when wound status was done. Patients were followed up at 6 weeks and scar assessment was done by interviewing patients and local examination of wound. Complications related to wound healing including infection, dehiscence, hematoma, and hypertrophic scar formation at sixth week of follow-up were noted, and cosmetic status of scar was assessed using Patient and Observer scar assessment scale (POSAS).([Figure 2]) [10]
Statistical analysis
All the data collected will be analysed using SPSS 24.0 software and relevant statistical techniques. Data was collected, compiled and presented in terms of percentages.
Approval by ethical committee
This study was conducted only after going through an internal mechanism of institutional ethical committee; involving the relevant specialist and administrative staff giving ethical approval. Written informed consent was taken from all patients.
Results
The present study was conducted in the department of Obstetrics and Gynaecology at tertiary care hospital, Amritsar from 1st January 2023 to 31 March 2024.
|
Age (in years) |
Monocryl |
|
≤ 20 |
03(2%) |
|
21 – 25 |
19 (12.7%) |
|
26 – 30 |
40 (26.7%) |
|
31 – 35 |
10 (6.7%) |
|
> 35 |
03 (2%) |
|
Total |
75 |
Mean age of study population was 27.40 ± 3.795 years.([Table 1])
|
BMI |
Monocryl |
|
< 18.5 |
12 (8%) |
|
18.5 – 22.9 |
57 (38%) |
|
23 – 24.9 |
02(1.3%) |
|
25 -29.9 |
04 (2.7%) |
|
Total |
75 |
57(38%) patients had BMI of 18.5 – 22.9 Kg/m2 and 12(8%) had BMI of <18.5 Kg/m2. The mean BMI for monocryl suture group is 21.492 +-3.987 Kg/m2.([Table 2])
|
Time for skin closure (mins) |
Monocryl |
|
4 |
14(9.3) |
|
5 |
33(22%) |
|
6 |
13(8.7%) |
|
7 |
7(4.7%) |
|
8 |
7(4.7%) |
|
9 |
1(0.7%) |
In 33 (22%) cases time of skin closure was 5 mins,14 (9.3%) had time of closure of 4 mins, 13 (8.7%) had time of closure of 6 mins and 8 had closure time of 7 mins. Mean time for skin closure was 4.96±1.382 mins.([Table 3])
|
Pain severity |
Monocryl |
|
Mild |
13(8.7%) |
|
Moderate |
57(38%) |
|
Severe |
05(3.3%) |
|
Total |
75(50) |
Out of 75, 57(38%) had moderate pain and 13(8.7%) had mild pain and 5(3.3%) had severe pain.([Table 4])
|
Pain assessment (NMS) score_5 Day |
Monocryl |
|
2 |
1 (0.7%) |
|
3 |
12(8.0%) |
|
4 |
10(6.7%) |
|
5 |
16(10.7%) |
|
6 |
31(20.7%) |
|
7 |
5 (3.3%) |
Majority 31(20.7%) cases were given score of 6 followed by 16(10.7%) who gave score of 5,10 gave score 4, 12 cases gave score of 3, 5 cases in monocryl group gave score 7 and only 1 gave score of 2. The mean pain score for monocryl was 5.05+ 1.451.([Table 5])
|
Complications |
Monocryl |
|
Hematoma |
2(1.3%) |
|
Hypertrophic |
3(2%) |
|
Dehiscence /Resuturing |
5(3.3%) |
|
Infection |
5(3.3%) |
|
Seroma |
9(6%) |
Seroma was present in 9(6%) cases, 5(3.3%) cases had infection, hematoma was present in 2(1.3%) cases, hypertrophy was present in 3(2%) cases and dehiscence was present in 5(3.3%) cases.([Table 6])
|
Total observer scar score |
Monocryl |
|
6 |
17(11.3%) |
|
7 |
22(14.7%) |
|
8 |
16(10.7%) |
|
9 |
4(2.7%) |
|
10 |
2(1.3%) |
|
11 |
1(0.7%) |
|
12 |
1(0.7%) |
|
>12 |
0(0.0%) |
Majority of the cases 22(14.7%) were given the score of 7 followed by score 6 in 17(11.3%) cases and 8 in 16(10.7%), 4 (2.7%) cases were given score of 9 and 2(2.3%) were given the total observer score of 10. The score of 11 and 12 were given to one (0.7%) each case. The mean observer scar score for monocryl was 6.173+-2.891. ([Table 7])
|
Total patient scar score |
Monocryl |
|
6 |
19(12.7%) |
|
7 |
13(8.7%) |
|
8 |
15(10%) |
|
9 |
5(3.3%) |
|
10 |
6(4%) |
|
11 |
4(2.7%) |
|
12 |
1(0.7%) |
In the present study, patient’s components were studied and total patient scar score was calculated based on the observation and score given by the patients at 6 weeks. The components of this score were pain, itching, stiffness, thickness, irregularity and colour of the scar. Majority of the cases 19(12.7%) gave the score of 6 followed by score 8 in 15(20%) cases and score 7 in 13(8.7%). 6 (4%) cases gave score of 10 and 5(3.3%) gave the total patient scar score of 9. The score of 11 was given in 4 (2.7%) cases while score of 12 was given by one (0.7%) case with no case having score greater than 12. The mean total patient scar score in case of monocryl sutures was 6.128 ± 1.291.([Table 8] )
Discussion
The present prospective comparative study was conducted in the Department of Obstetrics and Gynaecology at Sri Guru Ram Das Institute of Medical Sciences and Research, Sri Amritsar from January 2023 to March 2024. A total of 150 patients were enrolled for the study after going through the inclusion and exclusion criteria. Ethical Clearance from committee taken. Informed consent was taken from the cases. 12 cases lost to follow up. Despite the existence of conflicting viewpoints in the literature regarding the benefits and drawbacks of subcuticular closure, this method continues to be highlighted for its numerous advantages over alternative closure techniques. Various studies have elucidated its merits, particularly in terms of promoting optimal wound healing, yielding superior cosmetic outcomes, and enhancing overall patient satisfaction rates.[11]
As cited in numerous studies, suture closure stands out as the preferred approach for skin closure in caesarean incisions. However, there remains ongoing debate regarding the comparative benefits of subcuticular closure—whether employing absorbable or nonabsorbable materials—in relation to wound healing, aesthetic outcomes, and patient satisfaction. The POSAS provides a notable benefit by allowing for the integration of patient self-assessment regarding symptoms related to scarring and its physical attributes.[12]
In the present study mean age where Monocryl suture was used was 27.40 ± 3.795 years. The findings of the present study can be correlated with studies conducted by Tan et al, [13] Verma et al,[14] Hasdemir et al,[15] Poperzncy et al[16] and Kolaib et al.[17]
The mean BMI of study group was 21.492 +-3.987. In the study conducted by Tan et al[13] where mean BMI in non-absorbable sutures used was 26.7 ± 5.4 Kg/m2 and among the absorbable was 26.3 ± 4.2 Kg/m2. In another study by Verma et al[14] where mean BMI in females where absorbable suture was used was 27.24 ±4.48 Kg/m2 and among the non-absorbable suture was 28.38 ± 4.88 Kg/m2.
Study conducted by Hasdemir et al[15] used NRS pain scale to grade scar pain severity verbally on a scale of zero to ten scale ranging 1 to 10. No statistical difference between absorbable and nonabsorbable suture groups was found considering postoperative pain (p value-0.099).
The findings of the study can be compared with the studies conducted by Kolaib et al[17] where the mean time of closure 6.23 ± 4.58 for monocryl group and another study by Hasdemir et al[15] who observed that mean time for skin closure was 6.77 ± 1.12 for absorbable suture. Another study conducted by Poperenzcy et al[16] concluded that in group where absorbable sutures were used 10.43% cases had infection, 4% had hematoma.
Similar study conducted by Islam et al[18] showed that superficial wound infection/ seroma was observed in 0.35% in absorbable group and 0.34% in non-absorbable group. In a study by Yang et al[19] the patient component of the patient and observer scar assessment scale (POSAS) was used together with patient’s satisfaction regarding scar of cesarean section and their willingness for choosing the similar technique for skin closure in next cesarean section was asked. 52 had subcuticular closure where The PSAS score of mean, 21.8) was found.
Conclusion
In the present study Monocryl suture exhibited a notably shorter mean skin closure time and less wound pigmentation but was associated with elevated pain levels and increased complications such as seroma, hypertrophy, and dehiscence. However, the study's single-institutional nature and small sample size may limit generalizability, and the relatively short follow-up period of just six weeks might overlook long-term wound complications. Additionally, varying patient adherence to follow-up appointments introduced potential biases due to loss to follow-up. The reliance on subjective pain assessments further adds to the study's limitations. Future research is needed including RCT’s on multicentric levels with more extended follow-up periods and employing standardized, objective outcome measures to enhance the reliability and generalizability of findings across diverse patient populations and clinical contexts.
Source of Funding
None.
Conflict of Interest
None.
References
- Sana M. A Comparative Study of Skin Staples with Conventional Sutures for Abdominal Skin Wound Closures. . 2018. [Google Scholar]
- Buresch A, Arsdale A, Ferzli M, Sahasrabudhe N, Sun M, Bernstein J. Comparison of subcuticular suture type for skin closure after cesarean delivery: a randomized controlled trial. Obstet Gynecol. 2017;130(3):521-6. [Google Scholar]
- Hirko M, Lin P, Greisler H, Chu C. Biological Properties of Suture Materials. Wound Closure Biomaterials and Devices. 2018. [Google Scholar]
- Mackeen A, Devaraj T, Baxter J. Cesarean skin closure preferences: a survey of obstetricians. J Matern Fetal Neonatal Med. 2013;26(8):753-6. [Google Scholar]
- Daykan Y, Sharon-Weiner M, Pasternak Y, Tzadikevitch-Geffen K, Markovitch O, Sukenik-Halevy R. Skin closure at cesarean delivery, glue vs subcuticular sutures: a randomized controlled trial. Am J Obstet Gynecol. 2017;216(4). [Google Scholar]
- Buresch A, Arsdale A, Ferzli M, Sahasrabudhe N, Sun M, Bernstein J. Comparison of subcuticular suture type for skin closure after cesarean delivery: a randomized controlled trial. Obstet Gynecol. 2017;130(3):521-6. [Google Scholar]
- Martin D, Williams S. Medical applications of poly-4-hydroxybutyrate: a strong flexible absorbable biomaterial. Biochem Eng J. 2003;16(2):97-105. [Google Scholar]
- Selvi F, Cakarer S, Can T, Topcu S, Palancioglu A, Keskin B. Effects of different suture materials on tissue healing. J Istanb Univ Fac Dent. 2016;50(1):35-42. [Google Scholar]
- Mccaffery M, Beebe A. . Pain: Clinical Manual for Nursing Practice. 1989. [Google Scholar]
- Lenzi L, Santos J, Neto J, Fernandes C, Faloppa F. The Patient and Observer Scar Assessment Scale: Translation for portuguese language, cultural adaptation, and validation. Int Wound J. 2019;16(6):1513-20. [Google Scholar]
- Singer A, Hollander J, Quinn J. Evaluation and management of traumatic lacerations. N Engl J Med. 1997;337(15):1142-8. [Google Scholar]
- Kar A, Corion L, Smeulders M, Draaijers L, Horst C, Zuijlen P. Reliable and feasible evaluation of linear scars by the Patient and Observer Scar Assessment Scale. Plast Reconstr Surg. 2005;116(2):514-22. [Google Scholar]
- Tan P, Mubarak S, Omar S. Absorbable versus nonabsorbable sutures for subcuticular skin closure of a transverse suprapubic incision. Int J Gynaecol Obstet. 2008;103(2):179-81. [Google Scholar]
- Verma P, Ansari K. Comparison of Suture Materials in Caesarean Skin Closure. IOSR J Dent Med Sci (IOSR-JDMS. 2017;16(3):77-80. [Google Scholar]
- Hasdemir P, Guvenal T, Ozcakir H, Koyuncu F, Horasan G, Erkan M. Comparison of subcuticular suture materials in cesarean skin closure. Surg Res Pract. 2015;2015. [Google Scholar]
- Poprzeczny A, Grivell R, Louise J, Deussen A, Dodd J. Skin and subcutaneous fascia closure at caesarean section to reduce wound complications: the closure randomised trial. BMC Pregnancy Childbirth. 2020;20(1). [Google Scholar]
- Kolaib M, Mohamed W, Maaty A, Darwish R. Comparison between Subcuticular Skin Closure by Different Suture Materials in Cesarean Delivery: An Interventional Randomized Controlled Clinical Trial. Evid Based Women's Heal J. 2023;13(1):7-13. [Google Scholar]
- Islam A, Ehsan A. Comparison of suture material and technique of closure of subcutaneous fat and skin in caesarean section. N Am J Med Sci. 2011;3(2):85-8. [Google Scholar]
- Yang J, Kim K, Song Y, Kim S, Sung N, Kim H. Cosmetic outcomes of cesarean section scar; subcuticular suture versus intradermal buried suture. Obstet Gynecol Sci. 2018;61(1):79-87. [Google Scholar]
How to Cite This Article
Vancouver
Kaur S, Pahwa S. Monocryl 3-0 subcuticular in abdominal skin closure in cesarean sections [Internet]. Indian J Obstet Gynecol Res. 2025 [cited 2025 Nov 06];12(1):84-89. Available from: https://doi.org/10.18231/j.ijogr.2025.016
APA
Kaur, S., Pahwa, S. (2025). Monocryl 3-0 subcuticular in abdominal skin closure in cesarean sections. Indian J Obstet Gynecol Res, 12(1), 84-89. https://doi.org/10.18231/j.ijogr.2025.016
MLA
Kaur, Sukhmanjit, Pahwa, Sangeeta. "Monocryl 3-0 subcuticular in abdominal skin closure in cesarean sections." Indian J Obstet Gynecol Res, vol. 12, no. 1, 2025, pp. 84-89. https://doi.org/10.18231/j.ijogr.2025.016
Chicago
Kaur, S., Pahwa, S.. "Monocryl 3-0 subcuticular in abdominal skin closure in cesarean sections." Indian J Obstet Gynecol Res 12, no. 1 (2025): 84-89. https://doi.org/10.18231/j.ijogr.2025.016
