- Visibility 123 Views
- Downloads 33 Downloads
- Permissions
- DOI 10.18231/j.ijogr.2025.030
-
CrossMark
- Citation
Abstract
Background: Germ cell tumours (GCT) account for 15-20% of all ovarian tumours in children and the young female population. Mature cystic teratoma, commonly known as dermoid cyst, is the most common type of GCT. In this report, we are presenting a rare case of a totally detached mature cystic teratoma located in the pouch of Douglas, which posed a diagnostic challenge and was a wonder intraoperatively.
Case Report: A 41 year old woman, P2L2, came with a one year history of pain in the lower abdomen and distension of abdomen. Her initial ultrasound at an outside hospital showed uterine fibroids and features suggestive of bilateral endometrioma and underwent conservative management. However, her symptoms continued and she came to our hospital for further evaluation after 9 months. Repeat ultrasound showed multiple uterine fibroids and left endometriotic cyst, whereas CECT showed multiple fibroids and left dermoid cyst. She underwent laparotomy. Intraoperatively, the uterus showed serosal fibroids and a detached grape-like cystic mass approximately measuring 9 x 4 x 2cm lying in the pouch of Douglas and thus underwent total abdominal hysterectomy and bilateral salpingectomy along with en bloc removal of the cystic mass. Histopathology of the mass was suggestive of dermoid cyst.
In our present case, a diagnostic dilemma arose as the ultrasound imaging was reported as ovarian endometriosis, but she did not have symptoms suggestive of it. There are fewer reports regarding the detachment of the ovarian dermoid and its positioning in the pouch of Douglas. Thus, the explanatory theory behind it is an enigma.
Conclusion: Increased awareness among gynaecologists regarding such masses, coupled with thorough preoperative evaluation and intraoperative decisions, would provide proper justification for the patient’s management.
Introduction
Germ cell tumours (GCT) account for 15-20% of all ovarian tumours in children and the young female population.[1] Mature cystic teratoma, commonly known as dermoid cyst, is the most common type of GCT. Teratomas are tumours arising from pluripotent stem cells that have the capacity to differentiate into any of the three germ cell layers. Histologically, they are lined with stratified squamous epithelium with mature skin appendages found on their walls, and their lumen is filled with keratin, hair, sweat, and sebaceous glands and teeth.
In this report, we are presenting a rare case of a totally detached mature cystic teratoma located in the pouch of Douglas, which posed a diagnostic challenge and was a wonder intraoperatively.
Case Presentation
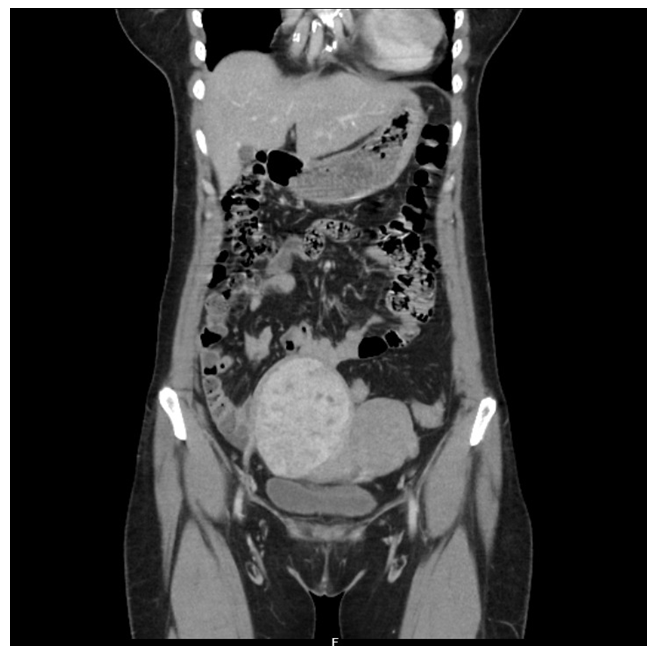
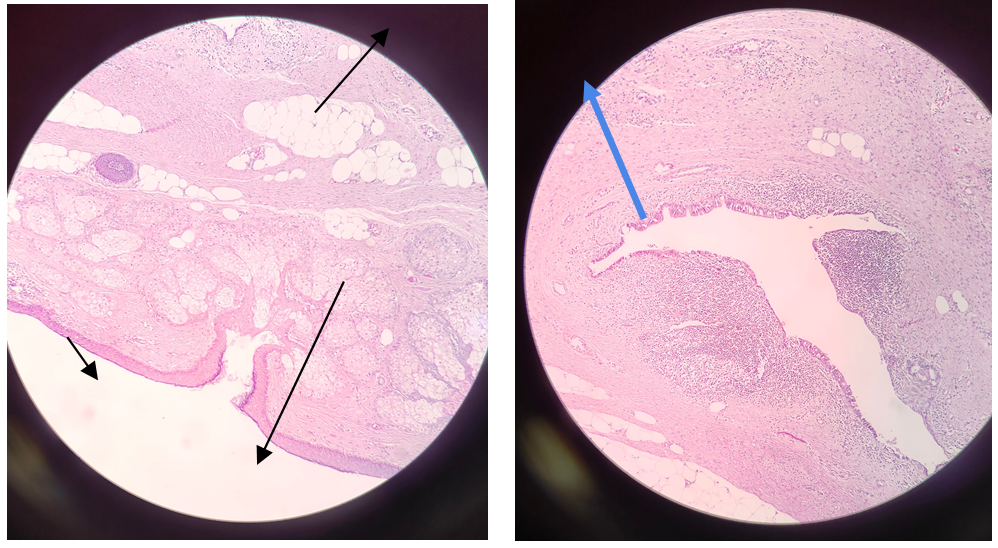
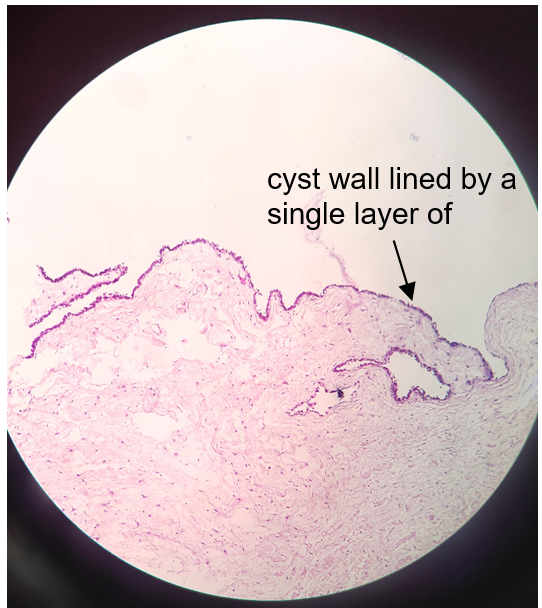
A 41 year old woman, P2L2, was admitted with a one year history of pain in the lower abdomen, with intermittent acute episodes that used to be relieved with analgesics. History of distension of abdomen was present for the past one year, and she was aware of its increasing size. The ultrasound initially done at an outside hospital on 1/6/2022 showed uterine fibroids and features suggestive of bilateral endometrioma. Hence, she was advised conservative management and received gonadotropin releasing hormone (GnRH) analogues (three doses of Inj. LEUPROLIDE 3.75mg IM) at an outside hospital. However, her symptoms continued, and hence came for surgical management at our hospital. The general condition was fair. On examination, a midline pelvi-abdominal mass corresponding to a 16-18 weeks gravid uterus with an irregular surface and firm consistency was noted. Tenderness was present over the supra-pubic, right iliac fossa (RIF) and left iliac fossa (LIF) regions. On bimanual examination, an enlarged uterus over 16-18 weeks in size was noted with restricted mobility and was non-tender. Right forniceal fullness and tenderness were present, while the left fornices were free and non tender. Pouch of Douglas fullness was also noted. The ultrasound at our hospital on 14/3/23 showed multiple uterine fibroids, with the largest in the subserosal fundal location measuring 7x6x10cm with bulky kissing ovaries in the midline, and a left ovarian cyst measuring 3.8 x 3 x 0.3cm showing low level internal echoes was identified and was suggestive of an endometriotic cyst. As her history was not suggestive of endometriosis, contrast enhanced computed tomography (CECT) was planned on 15/3/2023 to rule out any evidence of torsion, it showed multiple fibroids in the uterus, a cystic lesion measuring 9.5 x 5.7cm seen in the pouch of Douglas, showing fat density area measuring about 3 x 2cm, and a tiny calcific focus within the lesion ([Figure 1]). The left side ovary was not separately seen, and the right side ovary was normal, hence given the impression of a left dermoid cyst. Preoperative laboratory investigations were normal. CA 125 was 18.3U/mL and normal. Hence, she was planned for laparotomy, followed by total abdominal hysterectomy and left salphingoophoprectomy. Intra-operatively, the uterus corresponded to 12 weeks in size, with serosal fibroids identified in the fundal region (9 x 8 x 5cm) and the left lateral wall (6 x 5 x 4cm). A detached grape-like cystic mass measuring approximately 9 x 4 x 2cm was found lying in the pouch of Douglas and was subsequently taken out en-bloc ([Figure 2]). The left ovary showed a cyst measuring about 2 x 1.5cm, while the right ovary appeared normal. The bilateral fallopian tubes were morphologically normal. She hence underwent a total abdominal hysterectomy, bilateral salpingectomy, and left ovarian cystectomy. She remained uneventful in the post-operative period and asymptomatic. The histopathology of the multiloculated cyst showed pultaceous material with hair on gross examination of the detached specimen. Microscopy sections showed stratified squamous epithelium with pilosebaceous units, bronchial epithelium, adipose tissue, and areas of haemorrhage suggestive of dermoid cyst. Additionally, adjacent normal ovarian parenchyma was identified ([Figure 3]). The microscopy of the left ovarian cyst showed cyst wall lined by a single layer of flattened mesothelial cells, with bland ovoid to flattened nuclei with fibrous, edematous stroma, thus indicative of mesothelial inclusion cyst ([Figure 4]). The microscopy of the uterus was unremarkable, with secretory endometrium & features of leiomyomata in the myometrium.

Discussion
Mature cystic teratoma is a common germ cell tumour of the ovaries. In our present case, a diagnostic dilemma arose as the ultrasound imaging was reported as ovarian endometriosis. Our patient used to have recurrent acute episodes of pain abdomen to suggest chronic torsion, but she did not have dysmenorrhea and other symptoms suggestive of endometriosis. However, her ultrasound showed classic features of ovarian endometrioma, but her CECT confirmed the cystic lesion in the pouch of Douglas, suggesting a dermoid cyst. This turned out to be true intra-operatively, as a 9 x 4 x 2cm dermoid cyst was found detached in the pouch of Douglas, which was a peculiar and rare finding in our patient.
The dermoid cyst could be a gonadal teratoma that detached from the ovary through self amputation. Her experience of acute episodes of pain abdomen followed by relief after taking analgesics could suggest the possibility of undergoing autoamputation, as the histopathology examination of the detached mass showed features of a dermoid cyst with an ovarian parenchyma attached to it, and the origin could be ovarian, and then got autoamputated. However, the reason and process for autoamputation are difficult to explain. The torsion of the ovary may not be the cause for autoamputation as the adjacent structures were morphologically normal and showed no evidence of injury. The other origin could be from the extragonadal teratoma undergoing autoamputation. Finding the origin of the detached mass is a challenge. It could be of ovarian or extragonadal origin, as reported in literature. Kakuda et al.,[2] in their review of literature, states that six of the 19 cases were considered to result from auto-amputation, and nine of the 19 cases were considered to have an unknown etiology. Hence, distinguishing autoamputation from other causes, such as extragonadal de-novo generation from an ectopic ovary, as described by Wharton,[3] or from displaced primordial germ cells,[4] is quite challenging since the actual moment of auto-amputation is not observed.
There are fewer reports regarding the detachment of the ovarian dermoid and its positioning in the pouch of Douglas, which could be attributed to autoamputation. Thornton,[5] in 1881, was the first to suggest that extragonadal teratomas may undergo autoamputation into the abdominal cavity. Peh et al.[6] summarised 20 cases of autoamputated ovary in the literature, with 9 cases reported in the pelvis, including 1 case in the cul-de-sac as in our patient. Peitsidou A et al.[7] reported, during cesarean section at 39 weeks of gestation, an autoamputated dermoid cyst in the pouch of Douglas. In their 2017 study, Kim HG et al.[8] proposed that autoamputation could result from the torsion of the ovarian pedicle. Occasionally, the tumor completely detaches from its pedicle, leading to the formation of a parasitic dermoid cyst. Thus, the explanatory theory behind autoamputation is an enigma.
As the ovaries showed no evidence of dermoid, we assume a low recurrence chance, thus justifying the retention of ovaries in our patient. Our patient received thorough counselling regarding the same.
Conclusion
The detached mature cystic teratoma found lying in the pouch of Douglas with intact ovaries is a rare occurrence. Increased awareness among gynaecologists regarding such masses, coupled with thorough preoperative evaluation and intraoperative decisions, would provide proper justification for the patient’s management.
Source of Funding
None.
Conflict of Interest
None.
References
- Bhurgri Y, Shaheen Y, Kayani N, Nazir K, Ahmed R, Usman A. Incidence, trends and morphology of ovarian cancer in Karachi (1995-2002). Asian Pac J Cancer Prev. 1995;12(6):1567-71. [Google Scholar]
- Kakuda M, Matsuzaki S, Kobayashi E, Yoshino K, Morii E, Kimura T. A Case of Extragonadal Teratoma in the Pouch of Douglas and Literature Review. J Minim Invasive Gynecol. 2015;22(7):1311-7. [Google Scholar]
- Wharton L. Two cases of supernumerary ovary and one of accessory ovary, with an analysis of previously reported cases. Am J Obstet Gynecol. 1959;78:1101-19. [Google Scholar]
- Oosterhuis J, Stoop H, Honecker F, Looijenga L. Why human extragonadal germ cell tumours occur in the midline of the body: old concepts, new perspectives. Int J Androl. 2007;30(4):256-63. [Google Scholar]
- Thornton K. Dermoid cyst. Am J Obstet. 1881;19. [Google Scholar]
- Peh W, Chu F, Lorentz T. Painful right iliac fossa mass caused by a migrating left ovary. Clin Imaging. 1994;18(3):199-202. [Google Scholar]
- Peitsidou A, Peitsidis P, Goumalatsos N, Papaspyrou R, Mitropoulou G, Georgoulias N. Diagnosis of an autoamputated ovary with dermoid cyst during a Cesarean section. Fertil Steril. 2009;91(4):9-12. [Google Scholar]
- Kim H, Song Y, Na Y, Yang J, Choi O. A Rare Case of an Autoamputated Ovary with Mature Cystic Teratoma. J Menopausal Med. 2017;23(1):74-6. [Google Scholar]
How to Cite This Article
Vancouver
Mathew RA, Navada MH. Wonder of the wandering dermoid cyst [Internet]. Indian J Obstet Gynecol Res. 2025 [cited 2025 Sep 15];12(1):164-167. Available from: https://doi.org/10.18231/j.ijogr.2025.030
APA
Mathew, R. A., Navada, M. H. (2025). Wonder of the wandering dermoid cyst. Indian J Obstet Gynecol Res, 12(1), 164-167. https://doi.org/10.18231/j.ijogr.2025.030
MLA
Mathew, Reshma Ann, Navada, Mahesha H. "Wonder of the wandering dermoid cyst." Indian J Obstet Gynecol Res, vol. 12, no. 1, 2025, pp. 164-167. https://doi.org/10.18231/j.ijogr.2025.030
Chicago
Mathew, R. A., Navada, M. H.. "Wonder of the wandering dermoid cyst." Indian J Obstet Gynecol Res 12, no. 1 (2025): 164-167. https://doi.org/10.18231/j.ijogr.2025.030
